Ihr umfassender Leitfaden
Für die Behandlung des Sinus pilonidalis gibt es zwei Strategien, die jeweils Vor- und Nachteile haben und sich im Ablauf unterscheiden.
- Die minimal-invasive Behandlung (Pit Picking/Sinusektomie) ist ein kleinerer chirurgischer Eingriff, der ambulant in der Praxis mit lokaler Betäubung durchgeführt werden kann. Hierfür bieten wir den „All-in-one”-Termin an, bei dem die Operation direkt im Anschluss an die Untersuchung und das Beratungsgespräch erfolgen kann. Diese Methode eignet sich sowohl für Patienten mit nicht voroperierten Steißbeinfisteln als auch für Rezidive, sofern keine größeren Mittelliniendefekte vorliegen. Ein weiterer Vorteil der minimalinvasiven Operation ist, dass man sich für den seltenen Fall eines Rezidivs alle denkbaren Optionen offen hält.
- Die seitliche Verlagerung der Narbe (Karydakis-Operation) macht die Haarentfernung durch Rasur oder Laser weniger wichtig. Für diesen Eingriff ist ein separater Termin in einem ambulanten Operationszentrum unter Vollnarkose erforderlich. Diese Methode ist für die meisten nicht voroperierten Fisteln zu aufwendig. Diese Methode wird auch dann gewählt, wenn ein früherer chirurgischer Eingriff zu einem langwierigen und frustrierenden Heilungsverlauf geführt hat und der Patient eine Behandlung mit schnellem Abschluss wünscht. Alle Infos dazu gibt’s auf unserer Seite Karydakis-Operation.
Schritt 1: Diagnose Sinus pilonidalis

Schritt 2: Termin finden
Am einfachsten buchen Sie dafür hier direkt einen Termin in unserem Online Kalender:
- Die Diagnose ist klar und Sie wünschen Pit Picking OP direkt im Anschluß an Untersuchung und Beratung? Dann ist die Terminkategorie „Untersuchung/Behandlung Steißbeinfistel All-in-one“ für Sie gemacht. Sie buchen damit einen 2-stündigen Termin mit Behandlungsoption – eine große Erleichterung für all jene, die eine zweite Anreise vermeiden wollen und sich bereits einem Facharzt vorgestellt haben.
- Wenn Sie sich noch nicht sicher sind oder sich die Entscheidung in Ruhe überlegen wollen, empfehlen wir Ihnen, „Spezialsprechstunde Steißbeinfistel/Sinus pilonidalis“ zu wählen. Damit erhalten Sie einen 20-minütigen Termin zur Untersuchung und Beratung. Für die Operation vereinbaren wir dann einen Termin nach Ihren Wünschen. Ein solcher Beratungstermin ist auch unerläßlich, wenn eine Operation in Vollnarkose geplant werden soll, sei es auf Ihren Wunsch oder bei medizinischer Notwendigkeit.
Diese Termine bieten wir von Montag bis Freitag täglich an. Fast immer läßt sich innerhalb von 2 Wochen ein Termin finden. Bei akuten Schmerzen ist meist eine Vorbehandlung notwendig. Finden sie alle Informationen dazu auf der Seite Pilonidalabszess.
Bitte übermitteln Sie uns bei Buchung eines All-in-one Termins eine Fotodokumentation der betroffenen Stelle nach dieser Anleitung:
Fotodokumentation
Übersichtsbild
Fotodokumentation
Detailbild
Bitte beachten Sie, dass eine Untersuchung oder Behandlung bei anderen Diagnosen (Hämorrhoiden, Analfisteln etc.) an diesen Terminen nicht möglich ist, da die räumlichen und/oder personellen Voraussetzungen nicht gegeben sind.
Ein über unser Buchungssystem angefragter Termin wird vom Arzt erst bestätigt, wenn entweder der Patient bereits in unserer Praxis untersucht wurde oder vorab eine Bilddokumentation übermittelt wurden.
Schritt 3: Vorbereitung auf die Pit Picking OP
Vorerkrankungen: Teilen Sie uns bitte mit, wenn
- wesentliche Erkrankungen (Herz, Lunge, Blutgerinnung) bekannt sind
- Unverträglichkeiten und Allergien zu beachten sind (insbesondere Lokalanästhetika oder Antibiotika)
- Sie „blutverdünnende“ Medikamente einnehmen müssen
- oder Sie eine Vorbehandlung (z.B. Antibiotika bei Erkrankungen der Herzklappen oder Minirin bei angeborener Blutungsneigung) benötigen.
Fahrer / Begleitperson organisieren: Für die Heimfahrt empfehlen wir nicht, sich selbst ans Steuer zu setzen. Kreislaufreaktionen sind nie ganz auszuschließen. Direkt nach der Behandlung ist man vielleicht auch kein konzentrierter Teilnehmer im Straßenverkehr. Organisieren Sie also am besten einen Fahrer oder eine Anreise mit öffentlichen Verkehrsmitteln ohne allzu häufiges Umsteigen.
Schritt 4: Am Operationstag

Sie finden die Praxis Dr. Hofer / Liebl in der Brienner Straße 13 im 4. Stock über dem Café Luitpold im Zentrum von München. Der Eingang liegt zwischen Café und Blumengeschäft Flor&Decor.
Die U-Bahn hält direkt vor dem Haus (Haltestelle Odeonsplatz), ein Parkhaus befindet sich hinter dem Luitpoldblock.
Bitte beachten Sie, dass während der Rush Hour mit starkem Stadtverkehr und unerwarteten Umleitungen aufgrund zahlreicher Baustellen zu rechnen ist. Planen Sie daher ausreichend Zeit ein, um Stress zu vermeiden.

Sie müssen für die Sinusektomie, anders als bei Operation in Vollnarkose, nicht nüchtern sein. Essen und trinken Sie ausreichend. Gerade an heißen Sommertagen beugen Sie damit Kreislaufproblemen vor.
Diabetiker nehmen wie gewohnt ihre Mahlzeiten und Medikation zu sich.
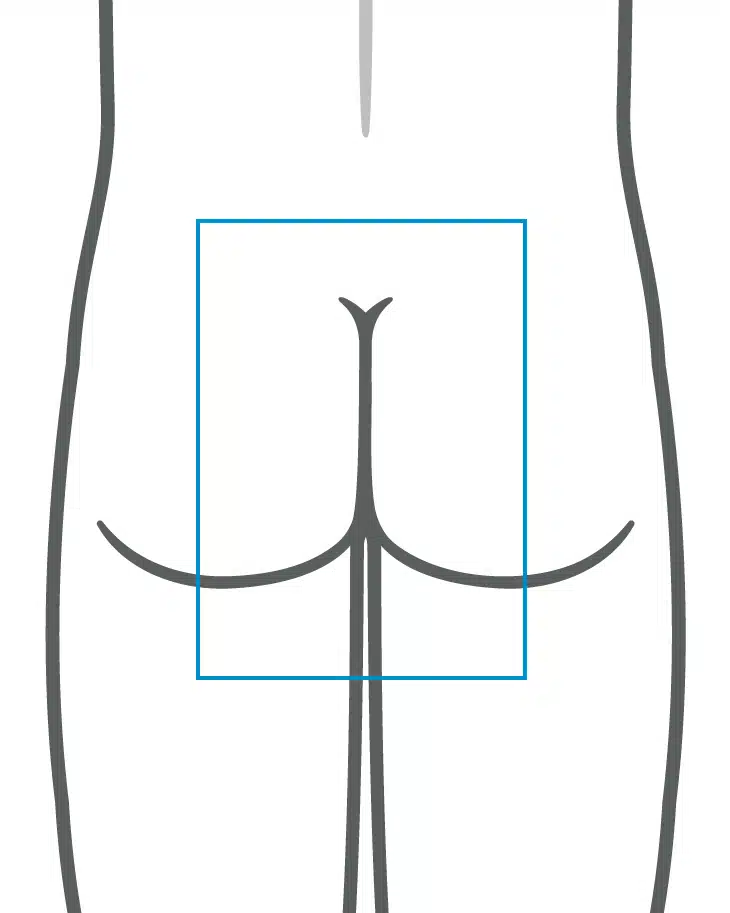
Wenn möglich, bitten wir das Gesäß großzügig zu rasieren. Das erleichtert uns die Arbeit und Ihnen die Verbandswechsel, wenn das Plaster nicht in den Haaren klebt.

Sie liegen auf einer extra dicken Gel – Matratze mit verstellbaren Kopfteil und verstellbaren Stützen für die Arme. Vor OP-Beginn empfiehlt es sich, noch einmal die Toilette aufzusuchen, dass es nachher nicht „drückt“.
Es folgen Rasur und örtliche Betäubung. Wenn möglich, können Sie die Rasur bereits zuhause erledigen, das spart etwas Zeit.
Typischerweise dauert der Eingriff zwischen 30 und 60 Minuten.
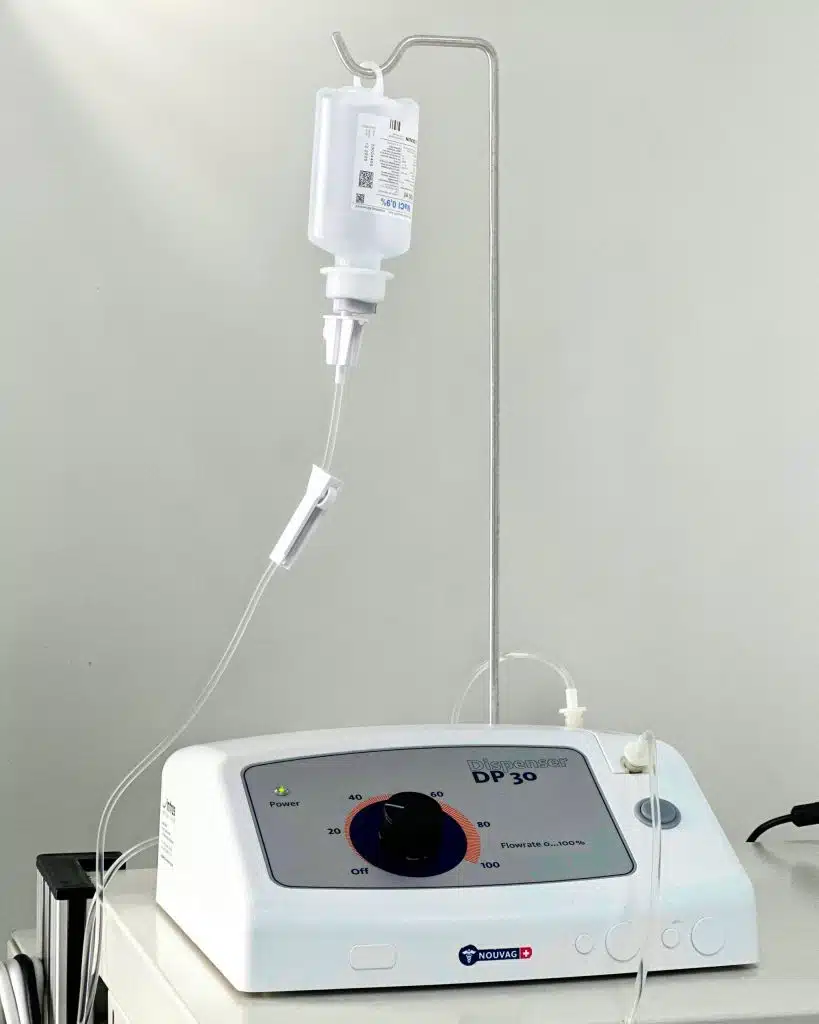
Lokalanästhetika werden seit 1884 in der Medizin eingesetzt und blockieren die Erregungsleitung in den Nerven. Dadurch ermöglichen sie eine schmerzfreie Operation bei normalem Bewusstsein. Viele Patienten befürchten, dass die Lokalanästhesie (örtliche Betäubung) nicht ausreichend wirkt. Es ist daher wichtig zu betonen, dass die Wirksamkeit und Sicherheit der Tumeszenzanästhesie durch zahlreiche Studien, u.a. durch Prof. Bussen an der Universität Würzburg, belegt wurden.
Diese Angst können wir Ihnen nehmen. Die Tumeszenzanästhesie (Tumeszenz lat. = Schwellung), 1985 vom Schönheitschirurgen Dr. Jeffrey A. Klein in USA entwickelt und seitdem in verschiedenen medizinischen Fachrichtungen erfolgreich angewendet, bietet viele Vorteile.
- auch große Areale können zuverlässig betäubt werden
- die Neigung zu Blutungen und Blutergüssen wird vermindert
- das Anästhetikum wirkt antibakteriell und beugt Infektionen vor
- die lange Wirkungsdauer gewährleistet Schmerzfreiheit auch im Anschluss an die Operation
- sie ist ein sicheres Verfahren, welches den Organismus weniger belastet als eine Vollnarkose
Welche Eingriffsformen lassen sich in diesem ambulanten Setting verantwortungsvoll durchführen?
Mit dem Laden des Videos akzeptieren Sie die Datenschutzerklärung von YouTube.
Mehr erfahren
Produktpräsentation Dermabond®, Herstellervideo von Ethicon
Offene Wundbehandlung
Kleine Wunden bis zu 1 cm lassen wir in der Regel offen. Eine herkömmliche Wundnaht ist in der Mittellinie oft nicht effektiv, da Scherkräfte, Bakterien und nachwachsende Haare die Heilung beeinträchtigen. Unter optimalen Bedingungen kann jedoch von diesem Grundsatz abgewichen werden, mit einer Erfolgsrate von etwa 80 % unter folgenden Voraussetzungen:
- Gute Gewebekonsistenz
- Ausschluss eines Abszesses
- Laserepilation vor dem Eingriff, um das Haarwachstum in den ersten zwei Wochen nach dem Eingriff bestmöglich zu reduzieren
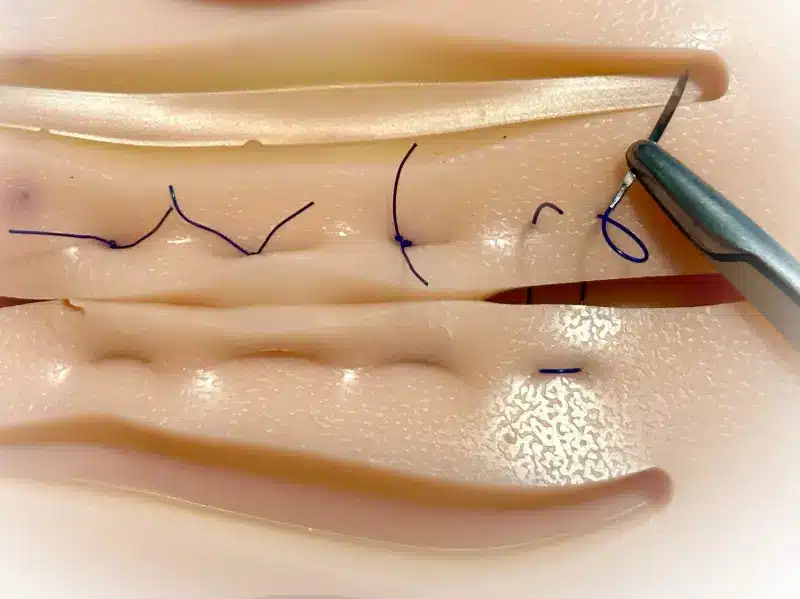
Wird die Wunde genäht oder geklebt?
Dabei kommen zwei verschiedene Techniken zum Einsatz:
- Wundklebung: Die Wundränder werden mit einer Art „Superkleber“ zusammengeführt und miteinander versiegelt.
- Eversionsnaht: Die Eversionsnaht ist eine Nahttechnik, die eine größere Kontaktfläche und eine bessere Durchblutung und damit Stabilität als eine Standardnaht bietet. Außerdem wird die Wuchsrichtung der Haare von der Wunde weg gelenkt.
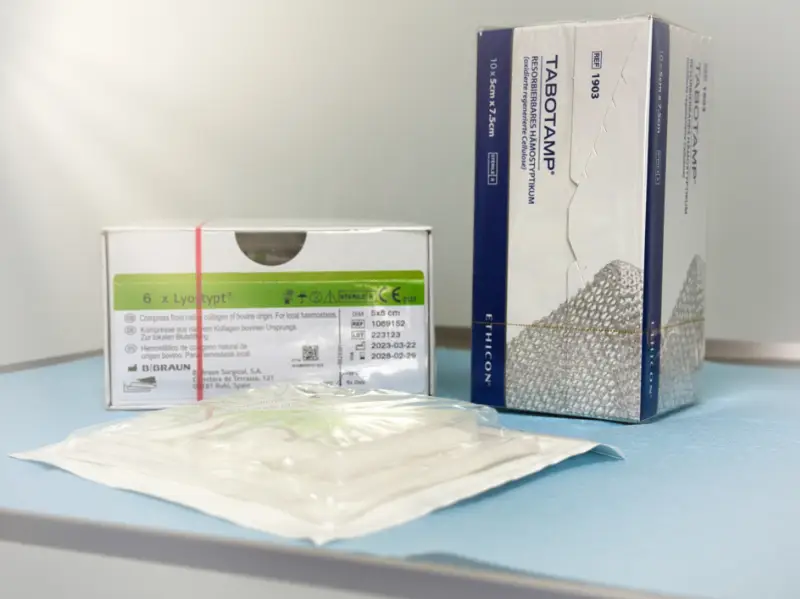
Verband und Tamponade
Wir legen in die Wundhöhle ein spezielles Flies, das als Hämostyptikum bezeichnet wird. Dieses Flies bietet zusätzlichen Schutz vor Nachblutungen, fördert die Wundheilung und löst sich im weiteren Verlauf vollständig auf. Diese Materialien enthalten Kollagen oder Gelatine tierischen Ursprungs. Sollten Sie – zum Beispiel aufgrund einer veganen Lebensweise – Bedenken haben, bitten wir um entsprechenden Hinweis.
Für den äußeren Bereich verwenden wir einen dicken Saugverband. Anfangs können Wunden oft größere Mengen Flüssigkeit absondern, und der Verband verhindert somit Flecken auf der Kleidung.
Mit dem Laden des Videos akzeptieren Sie die Datenschutzerklärung von YouTube.
Mehr erfahren

- Nachdem die Operation beendet und der Verband angelegt wurde, stehen Sie langsam von der Behandlungsliege auf, um Ihren Kreislauf zu stabilisieren.
- Wir bieten Ihnen eine Flasche Wasser, ein Gebäckstück und eine Schmerztablette an, während Sie sich im Wartebereich erholen.
- Nach einer abschließenden Verbandskontrolle und Kreislauf-Check können Sie die Praxis verlassen.
- Sollten Sie eine Bescheinigung hinsichtlich Arbeitsunfähigkeit oder für die Schule benötigen, informieren Sie uns bitte.
Schritt 6: Auf dem Heimweg
Nach dem Eingriff wirkt die Lokalanästhesie üblicherweise noch mehrere Stunden. Sie können und dürfen also schmerzfrei eine normale Sitzposition in Auto oder Zug einnehmen. Ein leichter Druck auf die Wunde ist sogar erwünscht und vermindert das ohnehin geringe Risiko einer Nachblutung.
Wir empfehlen nicht, sich selbst ans Steuer eines Kraftfahrzeugs zu setzen, da man in Gedanken vielleicht noch bei dem Eingriff ist und auch leichte Kreislaufreaktionen die volle Verkehrstüchtigkeit einschränken können.
Sie dürfen sich normal bewegen, am Operationstag selbst würden wir von längeren Märschen und Sport allerdings abraten.
Wenn es einmal blutet: Packen Sie mehrere Kompressen oder Zellstoffmaterial auf die Wunde und üben Sie für 15 Minuten konstant einen Druck aus. Hilfreich kann es auch sein, sich auf die Wunde zu setzen und etwas abzuwarten. Gefährlich ist eine Nachblutung nicht, im Zweifel kontaktieren Sie die Praxis oder die untenstehende Notfallnummer.
Schritt 7: Nachbehandlung

Den nach der Operation angelegten großen Verband können Sie selbst entfernen. Danach ist Duschen mit normalem Leitungswasser bei angenehmer Temperatur möglich und sinnvoll. Wir haben in der Vergangenheit noch nie negative Folgen gesehen. Nach den Hygienerichtlinien des Robert-Koch-Instituts (RKI) wäre ein endständiger Bakterienfilter („Legionellenfilter“, z.B. Germlyser D®) erforderlich, da nur sterile Flüssigkeiten an die Wunde gelangen dürfen. Der Bereich der Gesäßfalte ist jedoch nie steril und Waschen reduziert nachweislich die Keimzahl (Bundeszentrale für gesundheitliche Aufklärung).
Alltägliche Aktivitäten sind so weit wie möglich erlaubt. Extreme Spreizung des Gesäßes zur Begutachtung der Wunde sollte in den ersten 2 Tagen vermieden werden. Sport ist erlaubt, sobald der Wundschmerz es zulässt.
Wir empfehlen das Tragen einer eng anliegenden Unterhose mit einer handelsüblichen Slipeinlage. Diese Art der Wundversorgung ist angenehmer als ein aufgeklebter Verband. Die Wunde sondert blutiges Sekret ab. Der Wundschmerz ist am zweiten Tag stärker als am ersten und lässt im Laufe der Woche nach. Eine Behandlung mit Ibuprofen bei Bedarf ist praktisch immer ausreichend.
Schritt 8: Behandlungsabschluß und Rezidivprophylaxe

Das Hämostyptikum bzw. die Tamponade löst sich auf. Je nach verwendetem Material sieht das bei Tabotamp® bräunlich-breiig und bei Lyostypt® wie weisser Schaumstoff aus. Leichte Reizzustände und Schwellungen sind in dieser Phase normal.
Fibrin, ein natürlicher „Wundkleber“ aus Blutbestandteilen, bildet an Eiter erinnernde, gelbliche Beläge, muss Sie aber nicht beunruhigen.
Salben oder Puder sind normalerweise nicht nötig. Bei verzögerter Wundheilung verschreiben wir Salben mit Metronidazol, Mupirocin oder Jod (Betaisodona®), die Sie zweimal täglich auf die Wunde auftragen.
Einmal pro Woche ist es unbedingt erforderlich, die Wundränder mit einem Einwegrasierer zu rasieren und die Wunde auf eingedrungene Haare zu untersuchen. Dies kann durch uns, Angehörige oder den Hausarzt erfolgen. Bei gutem Licht und guter Sicht (evtl. Lupe, Lesebrille) wird die Wunde untersucht, Haare werden mit einer Pinzette entfernt. Nach Verschluss der Wunde sollte die Rasur noch 2 Monate fortgesetzt werden.
Zur Förderung der Wundheilunng haben wir verschiedene Optionen:
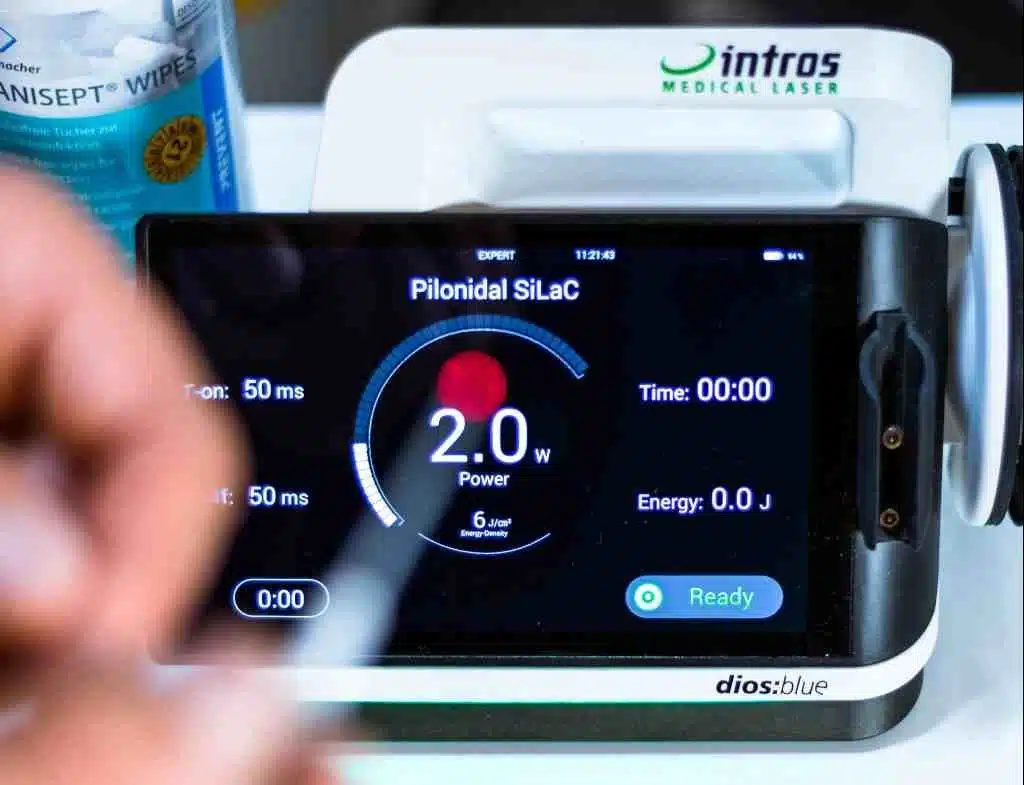
- Eine niederenergetische Laserbehandlung (“LLLT, Softlaser”) ein- bis zweimal wöchentlich regt über zelluläre Aktivierung die Selbstheilungskräfte an.
- Die Behandlung mit Kaltplasma (CAP) bewirkt eine hochwirksame Desinfektion bei gleichzeitiger Verbesserung der Mikrozirkulation.
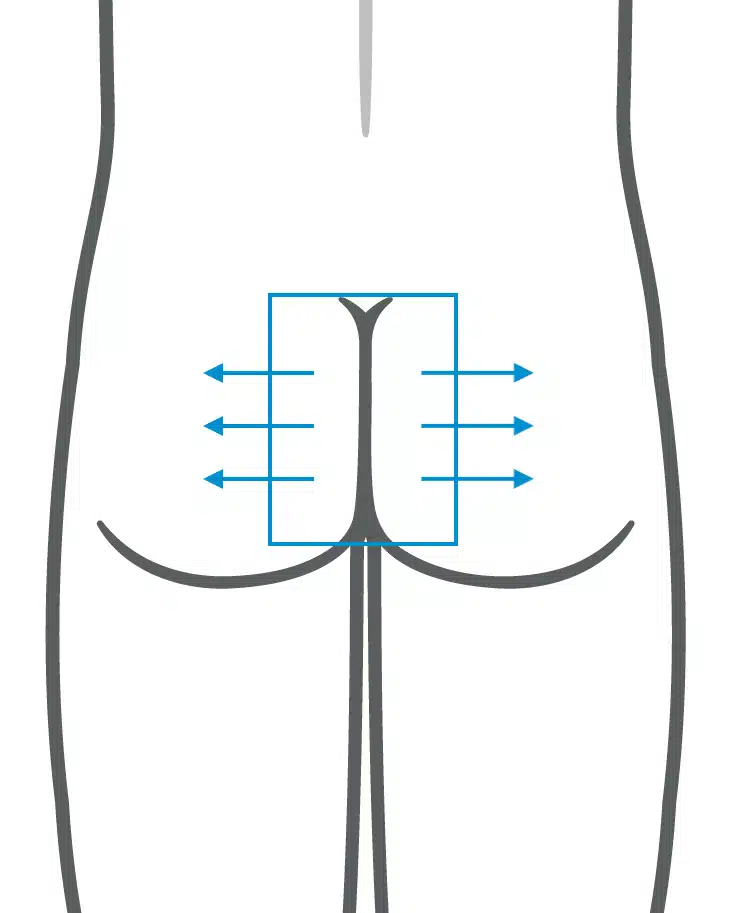
- Die Laserbehandlung zur Haarentfernung erfolgt alle 4-6 Wochen und ist eine vorbeugende Maßnahme gegen Rückfälle (Rezidive). Die Behandlung kann schmerzfrei unter örtlicher Betäubung durchgeführt werden.
Literatur zur Lokalanästhesie
Boeni, R. (2020). A Combined Prilocaine-Lidocaine Tumescent Solution Has Lower Clinical Side Effects Compared With Lidocaine Only. American Journal of Cosmetic Surgery, 37(3), 114-117.
Bussen, D., Sailer, M., Fuchs, K., & Thiede, A. (2003). Tumeszenz-Lokalanästhesie bei proktologischen Eingriffen. Der Chirurg, 74(9), 839-843.
Goyal, N. (2021). Tumescent anaesthesia for liposuction surgery—A review. Dermatological Reviews, 2(4), 180-187.
Holt, N. (2017). Tumescent anaesthesia: its applications and well tolerated use in the out-of-operating room setting. Current Opinion in Anesthesiology, 30(4), 518-524.
Piskin, T. (2009). Tumescent Local Anesthesia for Excision and Flap Procedures in Treatment of Pilonidal Disease. Diseases of the Colon & Rectum, 52(10), 1780-1783.
Klein, J. (1987). The Tumescent Technique for Lipo-Suction Surgery. The American Journal of Cosmetic Surgery, 4(4), 263-267.
Klein, J., & Langman, L. (2017). Prevention of Surgical Site Infections and Biofilms: Pharmacokinetics of Subcutaneous Cefazolin and Metronidazole in a Tumescent Lidocaine Solution. Plastic and Reconstructive Surgery Global Open, 5(5)
Lindenblatt, N., Belusa, L., Tiefenbach, B., Schareck, W., & Olbrisch, R. (2004). Prilocaine Plasma Levels and Methemoglobinemia in Patients Undergoing Tumescent Liposuction Involving Less Than 2,000 ml. Aesthetic Plastic Surgery, 28(6), 435-440.
Mantripragada, K., Yerke Hansen, P., Vazquez, O., Pires, G., & Becker, H. (2023). Pain Reduction Using Ropivacaine in Tumescent Solution following Lipoaspiration. Plastic & Reconstructive Surgery Global Open, 11(1),
Schöpf, E., et al. (2001) Tumeszenz-Lokalanästhesie: Ein neues Verfahren der Lokalanästhesie. Dtsch Arztebl 2001; 98(9): A-545 / B-459 / C-434
DR. BERNHARD HOFER & FLORIAN LIEBL
Fachärzte für Viszeralchirurgie und Proktologie – PartG mbB
Brienner Str. 13, D-80333 München
- info@darmsprechstunde.de
- Montag - Freitag: 08.00 - 13.00 und 14.00 - 18.00
- und nach Vereinbarung
- Samstag, Sonntag, Feiertag : geschlossen
- Beachten Sie auch unsere Hinweise im Titel dieser Website und auf unserer Telefonansage.
Mit dem Laden der Karte akzeptieren Sie die Datenschutzerklärung von Google.
Mehr erfahren
© 2024 Proktologische Praxis München