Der 6-Punkte Risikocheck
Die Beantwortung folgender Fragen kann Ihnen helfen, ein erhöhtes Risiko für eine Steißbeinfistel zu erkennen. Sollten Sie mehrere dieser Fragen mit ‚Ja‘ beantworten, empfehlen wir, dass Sie Ihren Arzt oder eine andere vertrauenswürdige Person bitten, die Gesäßfalte auf Anzeichen wie Schwellungen, Rötungen und insbesondere auf kleine Öffnungen zu untersuchen.
- Haben Sie eine starke Körperbehaarung?
- Ist bei nahen Verwandten eine Steißbeinfistel aufgetreten?
- Sitzen Sie oft viele Stunden ohne Pause?
- Haben Sie selten die Möglichkeit, sich gründlich zu waschen oder zu duschen?
- Sind Sie beruflich Haaren ausgesetzt, wie beispielsweise als Friseur oder im Kontakt mit Tierhaaren?
- Haben Sie Schmerzen beim Sitzen?
Schamgefühle sollten Sie nicht davon abhalten, bei Verdacht auf eine Steißbeinfistel professionelle medizinische Hilfe in Anspruch zu nehmen. Ihre Gesundheit verdient es. Im Frühstadium ist die Chance auf eine einfache Lösung des Problems am höchsten.

Sitzendes Leben: Gesundheitliche Risiken von Büro und Schulbank
Es mag dramatisch klingen, aber es ist tatsächlich ungesund, stundenlang ohne Pause zu sitzen. Diese Gewohnheit verursacht nicht nur Rückenschmerzen, sondern wirkt sich auch auf die allgemeine Gesundheit aus. Eine Auswertung von 27 großen Studien aus dem Jahr 2018 ergab ein erhöhtes Risiko für Herz-Kreislauf-Erkrankungen, Diabetes und sogar Tumoren des Darms und des Unterleibs sowie eine insgesamt verkürzte Lebenserwartung, je länger man täglich sitzt.
Und natürlich leidet auch der empfindliche Bereich der Gesäßfalte unter dem langen Sitzen. Die unvermeidliche, ständige Gewichtsverlagerung beim Sitzen kann in der Pofalte wie ein Förderband wirken, das unerwünschte Haare an unerwünschte Stellen befördert – ein potenziell schmerzhaftes Szenario.
Eine noch größere Bedeutung kommt dem Sitzen zu, wenn bereits eine unentdeckte Steißbeinfistel besteht. Durch den Druck beim Sitzen können die kleinen Fistelöffnungen (Pits) funktionell verschlossen werden, was zu schmerzhaften Entzündungen führen kann.

Sie fragen sich, was Sie tun können?
- Nutzen Sie einen höhenverstellbaren Schreibtisch am Arbeitsplatz, um zwischendurch auch im Stehen zu arbeiten und Ihrem Körper etwas Gutes zu tun.
- Gönnen Sie sich regelmäßige kurze Pausen, um sich zu bewegen und aufzustehen.
- Auf Reisen: Öfter mal an der Raststätte rausfahren und ein paar Schritte gehen und auch im Flugzeug nicht die ganze Strecke bis Thailand im der Touristenklasse eingepfercht sitzen bleiben!
- Telefonieren Sie im Stehen, um Ihre Muskeln zu aktivieren und Ihre Haltung zu verbessern.
- Nutzen Sie die Werbepausen beim Fernsehen, um aufzustehen, sich zu strecken und etwas zu bewegen.
- Bringen Sie sportliche Aktivitäten wieder in Ihren Alltag und spüren Sie die Energie, die Bewegung in Ihr Leben bringt.
- Lassen Sie sich von Apps für Smartphones und Smartwatches motivieren, sich mehr zu bewegen und Ihren Körper in Schwung zu bringen.
Viele Arbeitgeber haben erkannt, dass zumindest zeitweises Arbeiten im Stehen für die Gesundheit der Mitarbeiter vorteilhaft ist und stellen daher höhenverstellbare Tische zur Verfügung. Auch im Home Office ist es sinnvoll, über die Anschaffung eines solchen Tisches nachzudenken. Ein weiterer positiver Effekt besteht darin, dass es Hinweise darauf gibt, dass man kreativer und zielgerichteter arbeitet, wenn man nicht den ganzen Tag im Sitzen verbringt.
"Steißbeinkissen"
Das Steißbein ist mitnichten ein nutzloser Fortsatz der Beckenknochen. Zahlreiche Bänder und Muskeln setzen hier an. Fehlhaltungen führen zwar nicht unbedingt zur Steißbeinfistel, aber zu Schmerzen beim Sitzen. Geeignete Sitzkissen führen zu einer Umverteilung der Gewichtsbelastung und können solche Schmerzen lindern.
In der Nachbehandlung nach Steißbeinfistel OP kann ein solches Kissen das Sitzen erleichtern.
Tipps zur Körperhygiene bei Sinus pilonidalis
Allgemeine Körperhygiene
Eine Steißbeinfistel bekommt man normalerweise nicht, weil man sich zu wenig wäscht. Der tiefste Punkt der Gesäßfalte (in der Fachsprache: Rima ani) wird aber oft vernachlässigt. Sammeln sich hier Haarfragmente, können sie in die Haut einmassiert werden. Feuchtigkeit und abgeschilferte Hornschuppen der Haut bilden einen Nährboden für Bakterien und verstopfen erweiterte Poren. Also: beim Duschen eine Pobacke zur Seite halten und die Rima ani gründlich ausspülen.
Vorbeugung einer Entzündung

Steissbeinfistel und Sport
Trotz einer Steißbeinfistel ist es in vielen Fällen möglich, Sport zu treiben, solange bestimmte Vorsichtsmaßnahmen beachtet werden. Die Auswahl der Sportart spielt eine entscheidende Rolle. Sportarten, die wenig Druck und Reibung im Bereich des Steißbeins erzeugen, wie Schwimmen oder Radfahren, sind oft besser verträglich. Es ist jedoch ratsam, vor der Fortsetzung oder Aufnahme einer sportlichen Aktivität immer Rücksprache mit einem Arzt zu halten, um sicherzustellen, dass es in Ihrem individuellen Fall keine Risiken oder Bedenken gibt. Die richtige Pflege und Hygiene des betroffenen Bereichs sowie das Tragen lockerer, nicht einschneidender Kleidung können ebenfalls dazu beitragen, Beschwerden während des Sports zu minimieren. In jedem Fall ist es wichtig, auf Ihren Körper zu hören und bei Schmerzen oder Problemen sofort einen Arzt zu konsultieren.
Schwitzen
Obwohl es immer wieder behauptet wird, gibt es keine Beweise dafür, dass Schweiß eine Rolle bei der Entstehung des Sinus pilonidalis spielt.
Schwitzen ist ein lebenswichtiger Mechanismus des menschlichen Körpers, um die Körpertemperatur zu regulieren und überschüssige Wärme abzuleiten. Die Schweißproduktion wird durch verschiedene Faktoren wie körperliche Aktivität, Umgebungstemperatur, Emotionen und den allgemeinen Gesundheitszustand reguliert.
Schweiß besteht hauptsächlich aus Wasser, Elektrolyten wie Natrium und Kalium sowie geringen Mengen an Harnstoff, Milchsäure und auch Immunglobulin A.
IgA dient dem Schutz von Haut und Schleimhäuten vor Mikroorganismen. Es besitzt die Fähigkeit, Toxine zu binden und entwickelt in Kombination mit Lysozym antibakterielle und antivirale Eigenschaften.
Und was ist nun mit der Wundheilung? Nun, da gibt die Wissenschaft noch keine klare Antwort. Ein saurer pH-Wert und IgA in unserem Schweiß könnten Wunden tatsächlich vor Infektionen schützen. Derzeit wird sogar untersucht, ob synthetischer Schweiß die Wundheilung verbessern kann.
Wer schwitzt, kurbelt darüber hinaus die Durchblutung an und gibt dem Heilungsprozess den nötigen Kickstart.
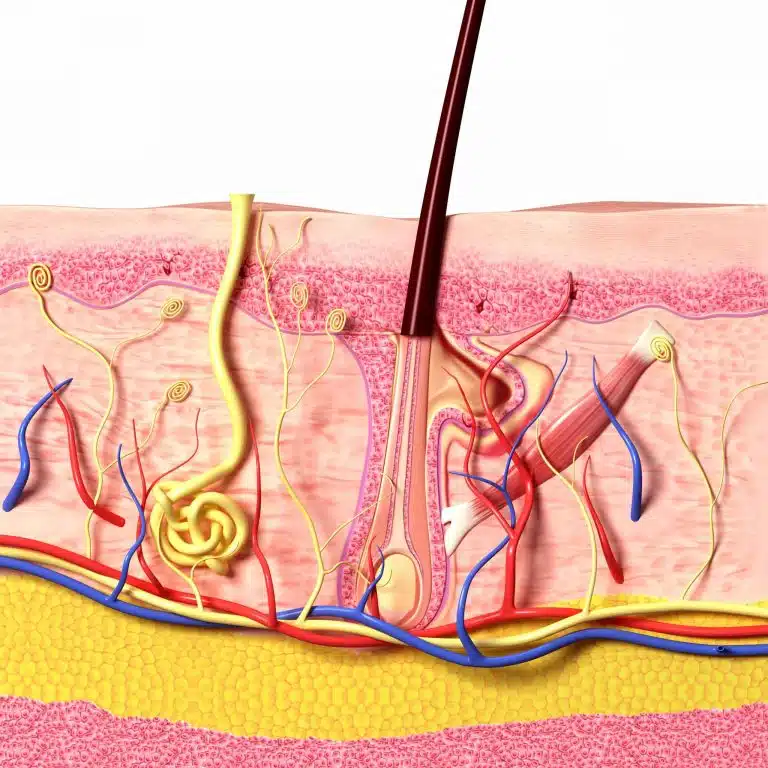
Reibung und textile Fasern
Es gibt die Theorie, die besagt, dass auch Textilfasern durch Reibung und Druck in die Hautporen eindringen können. Diese eingedrungenen Haare und Fasern könnten eine Fremdkörperreaktion auslösen, die zu einer Entzündung führt und schließlich die Bildung eines Pilonidalsinus zur Folge hat. Allerdings gibt es bislang keine systematischen Studien, die diese Annahme unterstützen. Zudem konnte ich in den annähernd 7000 Pilonidalfisteln, die wir bisher operiert haben, nie Textilpartikel identifizieren, die mit dem bloßen Auge oder unter Verwendung einer Lupenbrille sichtbar gewesen wären. Staub und Fusseln scheinen also nicht die Übeltäter zu sein.
Vorbeugende Laser-Behandlung?
Wenn Sie eine Steißbeinfistel ganz verhindern wollen, müssten Sie früh anfangen. Wahrscheinlich entstehen die ersten „pits“ schon ab Beginn der Pubertät. Unsere jüngsten Patienten sind kaum älter als 13 Jahre.
Eine frühzeitige, dauerhafte Entfernung der Haare der Gesäßfalte durch Laser wäre unter Umständen eine kausale Behandlung. Leider läßt sich nicht zuverlässig abschätzen, welcher junge Mensch von einer Laserepilation profitieren würde. Die Laserepilation wird von gesetzlichen Kassen nicht übernommen. Es sind immer mehrere Behandlungen notwendig. Eine rein vorbeugende Laserepilation scheint mir daher nur gerechtfertigt bei sehr ausgeprägter Behaarung oder mehreren von einer Steißbeinfistel betroffenen Familienmitgliedern.
Publikationen zum Thema Lifestyle
Biddle, S., Bennie, J., Bauman, A., Chau, J., Dunstan, D., Owen, N., Stamatakis, E., & van Uffelen, J. (2016). Too much sitting and all-cause mortality: is there a causal link?. BMC Public Health, 16(1), 1-10.
Dunstan, D. (2010). Too Much Sitting The Population Health Science of Sedentary Behavior. Exercise and Sport Sciences Reviews, 38(3), 105-113.
Eanes, L. (2018). CE: Too Much Sitting: A Newly Recognized Health Risk. AJN: American Journal of Nursing, 118(9), 26-34.
Kennedy, M. (2018). Sitting Our Lives Away. AJN The American Journal of Nursing, 118(9)
Pronk, N. (2011). The Problem With Too Much Sitting A Workplace Conundrum. ACSM’s Health & Fitness Journal, 15(1), 41–43-41
Wallace, J. (2015). Effect of Prolonged Sitting and Breaks in Sitting Time on Endothelial Function. Medicine & Science in Sports & Exercise, 47(4), 843–849-843
Unsere Empfehlungs-Ampel
DR. BERNHARD HOFER & FLORIAN LIEBL
Fachärzte für Viszeralchirurgie und Proktologie – PartG mbB
Brienner Str. 13, D-80333 München
- info@darmsprechstunde.de
- Montag - Freitag: 08.00 - 13.00 und 14.00 - 18.00
- und nach Vereinbarung
- Samstag, Sonntag, Feiertag : geschlossen
- Beachten Sie auch unsere Hinweise im Titel dieser Website und auf unserer Telefonansage.
Mit dem Laden der Karte akzeptieren Sie die Datenschutzerklärung von Google.
Mehr erfahren
© 2024 Proktologische Praxis München

