Important facts about sinus pilonidal surgery
The 3 most common surgical techniques
The majority of surgeons almost everywhere in the world recommend radical (from the Latin radix = root) excision of the Pilonidal Sinus. although a recurrence rate of up to 57 % is stated for this (Deutsches Ärzteblatt 2019). The guideline still refers to this procedure as the standard. We do not perform this surgery because we are convinced that there are good alternatives.
Karydakis OP and Limberg OP are techniques of plastic closure. This does not mean closing the wound with plastic. Rather, tissue from the area surrounding the wound (the "flap") is mobilized so that suture closure is possible. Consequently, these techniques are also called flap plastic surgery.
Pilonidal Sinus Operations
pit picking | FiLaC/SiLaC | Sinusectomy | Radical Excision | Karydakis | Limberg | |
|---|---|---|---|---|---|---|
Availability | Special practice/clinic | Special practice/clinic | Special practice/clinic | General Surgeon | Special practice/clinic | Special practice/clinic |
Inpatient/outpatient | outpatient | outpatient/inpatient | outpatient/inpatient | stationary | stationary | stationary |
Type of anaesthetic* | LA | LA/ITN/SPA | LA/ITN/SPA | ITN/SPA | (LA)/ITN/SPA | ITN/SPA |
OP Duration | 20 min | 20 - 30 min | 30 - 120 min | 30 min | 40 - 90 min | 40 - 90 min |
Disability | 0 - 2 weeks | 0 - 2 weeks | 2 - 3 weeks | 1 - 12 months | 4 weeks | 4 weeks |
* SPA = spinal anaesthesia, spinal cord anaesthesia, ITN = intubation anaesthesia, general anaesthesia, LA = local anaesthesia, local anaesthetic.
Table: Overview of the most common techniques used in Pilonidal Sinus surgery.
This assessment is based on my personal experience with the patients presented in our practice. It is subject to a selection effect and a certain subjectivity. Conventionally operated patients will only seek a second opinion if there are problems in the course of wound healing or if a relapse occurs, and are thus disproportionately represented in our collective.
My evaluation of the methods of Pilonidal Sinus surgery ranges from 0 stars (not recommendable) to 5 stars (method of first choice). From our point of view, the recommendable methods are marked with a green light, conditionally suitable methods with a yellow light, and less recommendable methods with a red light.
The conventional operation: Radical excision ("Metzger method")
Large-area removal with open wound treatment
Historical development
Based on the assumption of a congenital malformation, a radical (lat. radix = root) excision of the fistula-bearing tissue has been demanded since the beginning of the 20th century. In order to avoid recurrences, a "safety margin" of healthy tissue was also removed. Thus, no relapses (recurrences) could have occurred with complete removal.
But there were relapses nevertheless!
Thus the theory of a disease existing from birth had to be questioned. The obvious consequence of reconsidering the surgical procedure was not generally drawn. The Chief of Staff of the American armed forces had already banned the radical operation after it had brought 79,000 soldiers into inpatient treatment for an average of 55 days (Jeep rider's disease).
Instead, new justifications for the radical operation were found. The resulting extensive scar was supposed to protect against the re-growth of hair by keeping the hair free.
And then? How can a wound closure be achieved?
Basically, there are 3 possibilities: open wound treatment, the hardly used hemming of the wound edges to flatten the wound (marsupialisation) and the closure of the wound by suture.
Open wound treatment
What is meant by this is not rare: We'll see. The 5-10 cm long and 3 - 5 cm wide wound should fill with scar tissue. To avoid premature closure, the wound cavity is stuffed with a tamponade.
There are two ways of wound healing: Primary wound healing occurs when the edges of the wound are in close contact, e.g. in a sutured wound. First, it sticks together with fibrin, a protein from coagulation factors in the blood. The scar gains firmness in the second step when connective tissue cells multiply and form stable collagen fibres.
After the radical excision only secondary wound healing is possible. First the wound cleans itself. Then it fills with granulation tissue. When the skin level is reached, new skin grows over the scar in a final step.
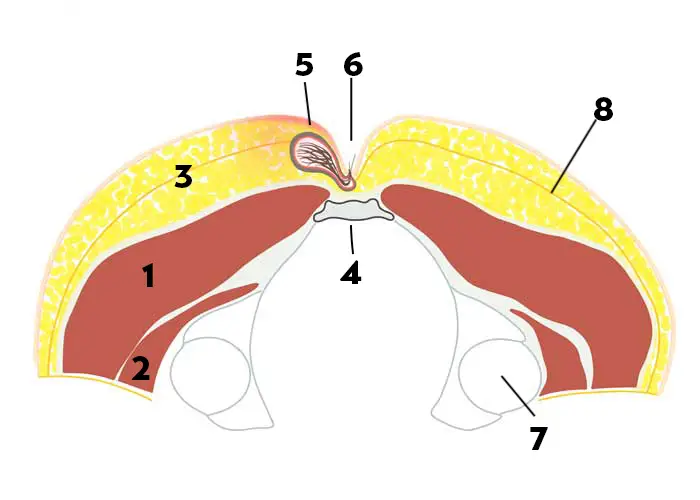
In case of secondary wound healing, physical protection is of no use. Wound infections are rare. In the coccyx region, regrowing hair and loose hair from other parts of the body as well as textile particles from clothing are the most frequent disturbing factors. We have already found hair from other family members and pets in non-healing wounds at Pilonidal Sinus .

Seam closure in the center line - usually not a good idea
It would be an obvious thought to sew up the wound. Especially with a small wound one could imagine that.
Unfortunately, the suture in the midline heals without problems only in part of the cases.
Regrowing and loose hairs penetrate the sutured wound, the stitches hinder the necessary shaving.
Moisture and bacterial colonisation favour wound infections. The suture bursts open again or must be opened prematurely.
Shear forces and constant movement cause the seams to become loose.
For these reasons, techniques that attempted to compensate for the loss of soft tissue by mobilizing fatty tissue(flapplasty according to Maruyama) were not successful because the wound was ultimately closed in the midline.
Suturing in the midline is not recommended in the current guideline. In well justified individual cases, such a suture can nevertheless help to shorten the healing time. From my experience, the prerequisites are
- inflammation-free conditions during the operation
- Treatment with laser epilation on the day of surgery
- meticulous removal of hair in the wound area 1 - 2 times a week
- early suture removal around the 10th day after surgery

How the wound can look like after such an operation, you can see for example on this page of an affected person
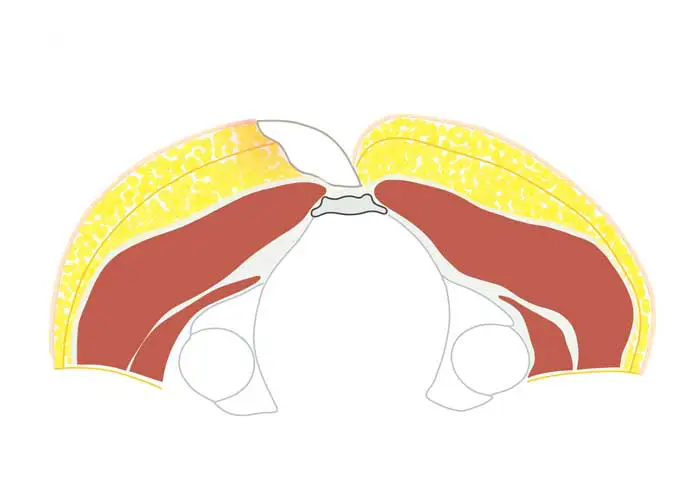
Operation procedure Radical surgery ("Excision in toto")
- Usually surgery under general or spinal anaesthesia (spinal anaesthesia)
- Mostly in-patient surgery performed in hospital as an in-patient.
- The sleeping patient is first turned into the prone position. The skin is disinfected and the surrounding area sterilely covered.
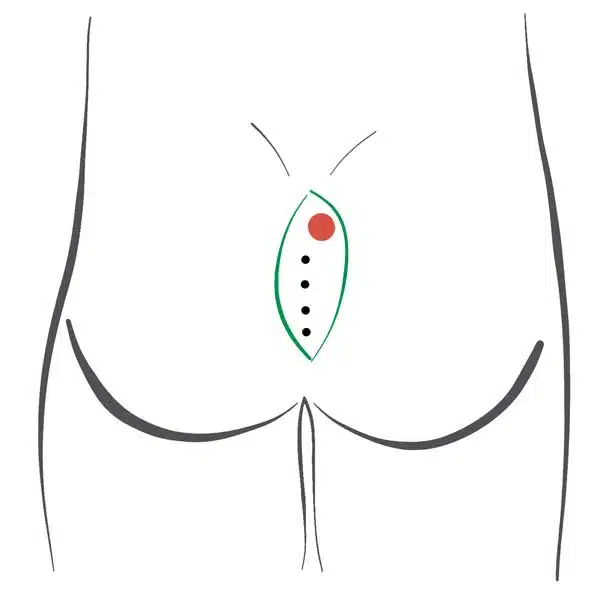
- Most surgeons first inject a blue dye to be able to recognize the dimension of the fistula by the blue coloration.
- Using a scalpel or electric knife, a spindle-shaped ("whetstone") block of tissue is cut out "safely in the healthy" down to the periosteum (fascia).
- The wound remains open. Tamponade (stuffing of the wound) is often carried out with sterile compresses or iodoform-soaked textile strips.
- These tamponades are changed regularly. Patients are usually instructed to wash out the wound regularly.
- Pilonidal Sinus Op Duration: 20 - 30 minutes
Here you can find a Video of conventional cutting. Formulations of the operation protocol can be found, for example, in OP-Bericht.de.
Radical surgery - when do we use the method?
- at typical Pilonidal Sinus: Never
- inversa acne: when conservative therapy and minimally invasive surgery have not been successful
Pro
- Simple surgical technique
- available nationwide
- complete fistula removal easy to achieve
Contra
- major wound
- protracted healing
- unfavourable scars
- high rate of failure to heal
- high recurrence rate
Operation after Karydakis: Lateral wound closure
Plastic reconstruction
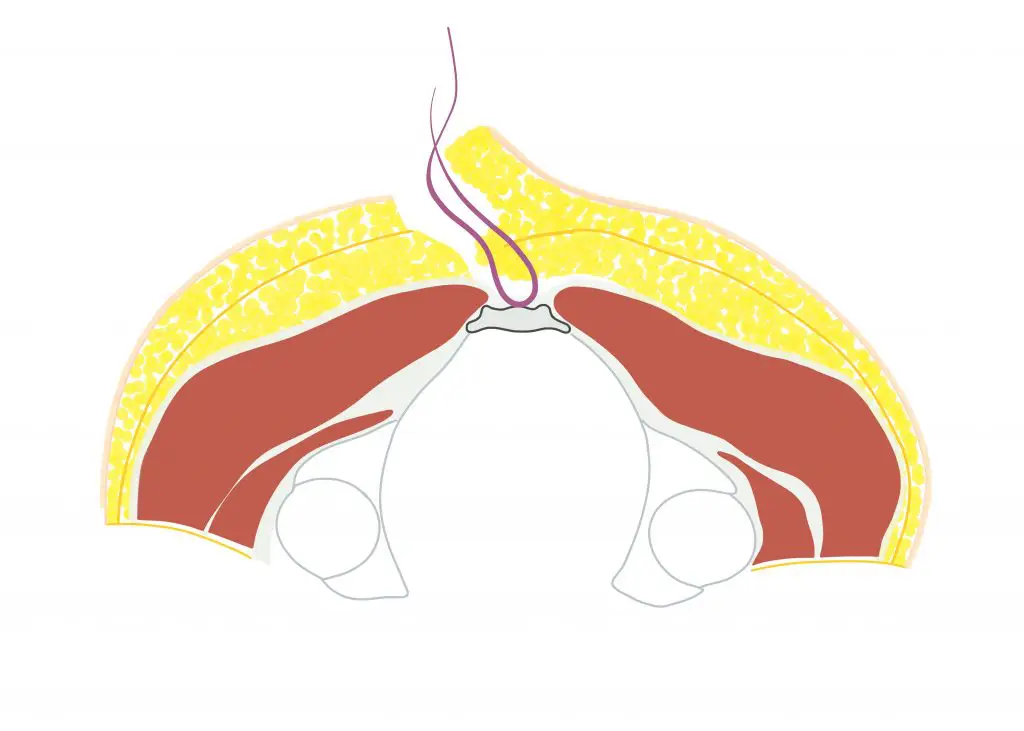
This technique goes back to the Greek military surgeon George E. Karydakis back. He recognized the problem of difficult healing and high recurrence rate. With his 1974 published technique of a laterally (laterally) displaced incision and reconstruction of the wound in 1974, he significantly improved the results of Pilonidal Sinus surgery.
Operation procedure Karydakis OP
- General or spinal anaesthesia (spinal anaesthesia)
- Inpatient treatment and abdominal positioning
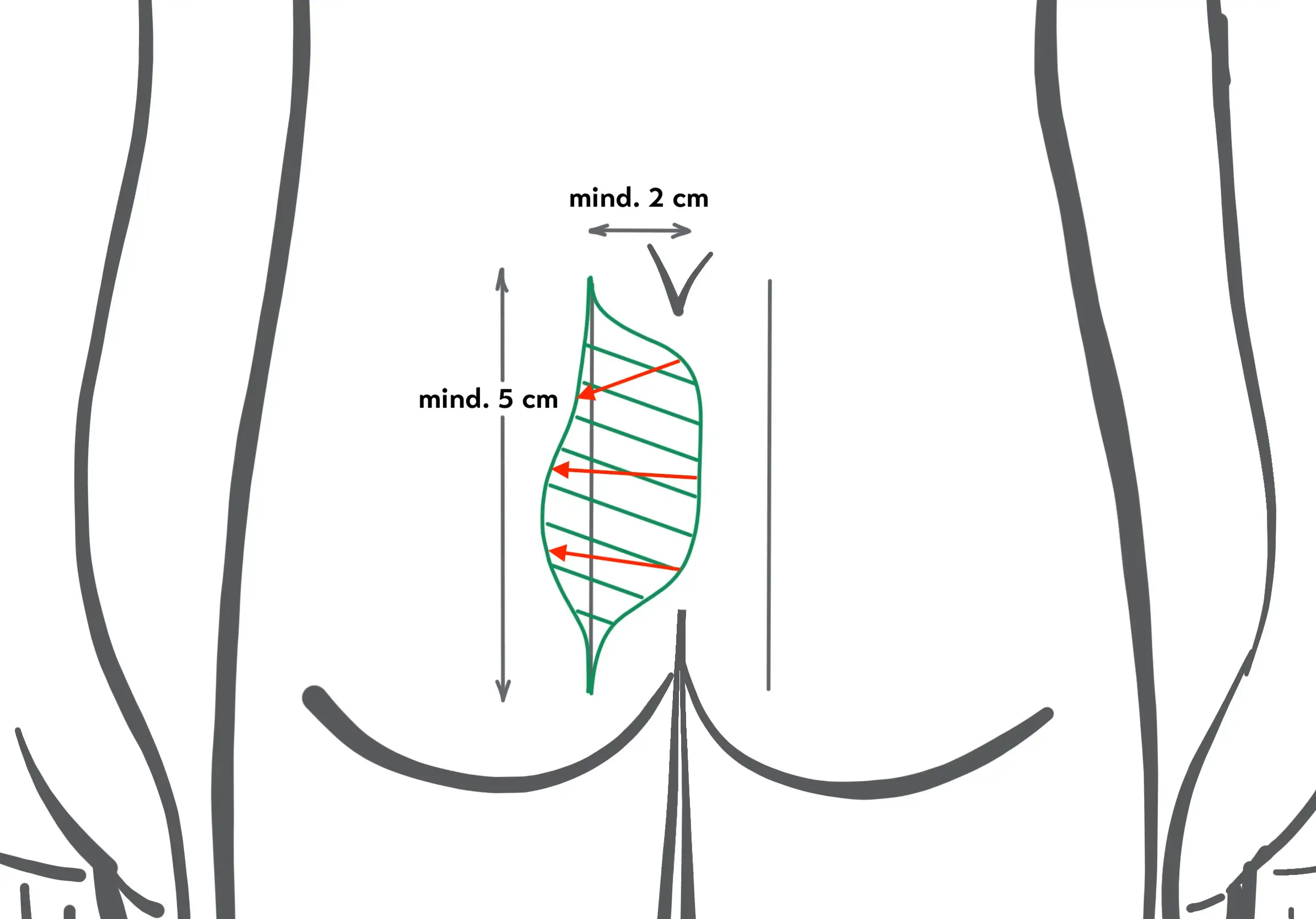
- The cut-out is made offset to the side. The length of the cut is at least 5 cm.
- Closure by suture is achieved on the side "lateralised", "off-midline" - at least 2 cm to the side of the midline - and with flattening of the gluteal fold.
- A suction drainage (Redon) can be inserted.
- 3 weeks are indicated to take iteasy .
- If the course is uncomplicated, healing is then achieved. The flattening of the gluteal fold should prevent relapses.
- You can change the course of the operation, for example, to www.webop.de understand.
Karydaki's surgery - when do we use the method?
- with typical, not pre-operated Pilonidal Sinus: Rare
- for acne inversa: very rare
- in case of recurrence after radical surgery, if minimally invasive surgery has not been successful
Pro
- Even large defects can be closed
- Very good recovery rates: Karydakis itself indicates a recurrence rate of 1%, a complication rate of 8.5% and a follow-up rate of 95% for 6545 patients operated on in 24 years!
- Low recurrence rate (0 - 6 %) due to lateral scar and flattening of a deep gluteal fold
Contra
- Technically demanding operation, experienced surgeon required
- Even with optimal OP technique 8 - 23 % haematomas (bruises) and wound healing disorders
- Seroma formation possible (fluid accumulation under the scar)
- Bei Wunden sehr nahe des Afters (< 2 cm Abstand zur Anokutanlinie) nicht anwendbar
- Visible scar, Altered body contour
Author | Year | Quantity | % Follow up | Years Follow up | % Recurrence | % Complication |
|---|---|---|---|---|---|---|
Petersen | 2006 | 97 | 100 | 0,8 | not reported | 21 |
Bessa | 2013 | 125 | 96 | 20,5 | 2 | 23 |
Cleft lift to Bascom: Modification of Karydakis surgery
Plastic reconstruction
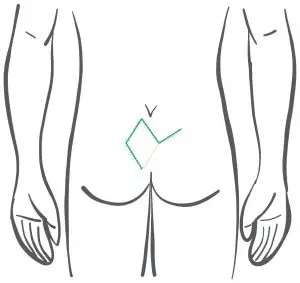
This technique is similar to the Karydakis operation in terms of the incision and the concept of lateral wound closure.
This technique focuses on the entry point for hair and bacteria. The fistula is not necessarily excised to its depth, but only unroofed and "cleaned out". The mobilized tissue, the "flap" comprises only the skin and a thin layer of subcutaneous tissue and is therefore thinner and easier to suture.
Descriptions of the technique in different variants can be found at Bascom and Favuzza, among others. From my point of view it is not conclusively clarified whether the fistula capsule does not represent a reservoir of firmly ingrown hairs and bacterial colonization which should better be removed.
Author | Year | Quantity | % Follow up | Years Follow up | % Recurrence | % Complication |
|---|---|---|---|---|---|---|
Bascom | 2002 | 31 | 87 | 1,67 | 0 | 9,6 |
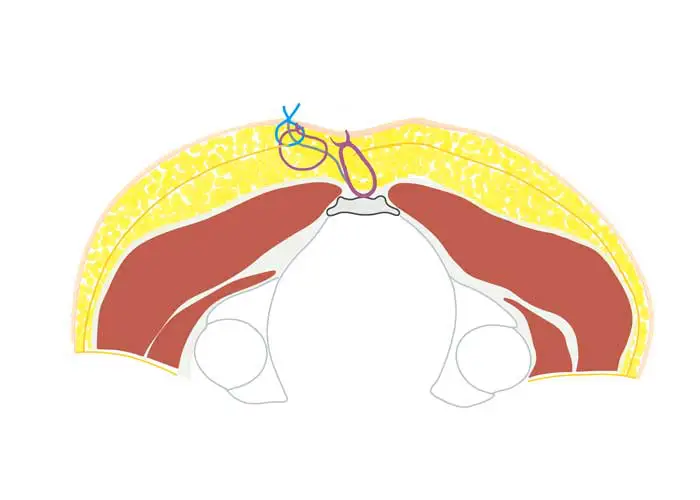
Limberg - Operation: Closure by rotation flap
Plastic reconstruction
This technique goes back to the Russian oral surgeon Alexander A. Limberg who published a technique for closing a diamond (rhombus) shaped defect in Russian in 1948 and in English in 1966. In 1984 this technique was published by A.S. G. Azab first used in Egypt to close a coccyx fistula wound. The description of the Limberg operation below follows this publication.
Apart from the Karydakis operation, Limberg plastic surgery is the most frequently used procedure with plastic wound closure. Excellent results are reported. Unfortunately, we often see patients in our consultation who have had complicated recurrences despite (or precisely because of?) an extremely extensive operation. Various modifications of this technique have been described, such as the Dufourmentel and Leaf Flap.
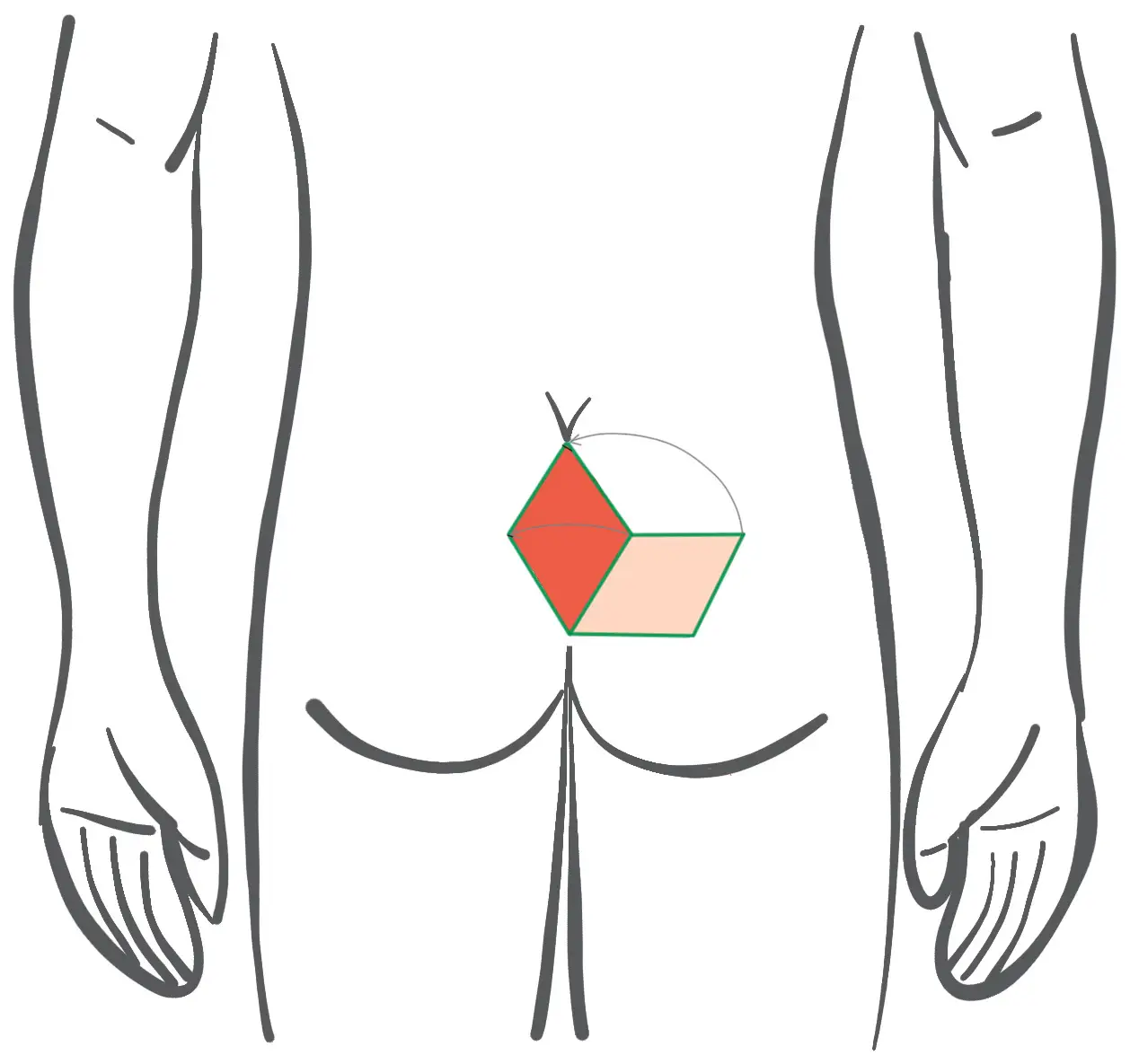
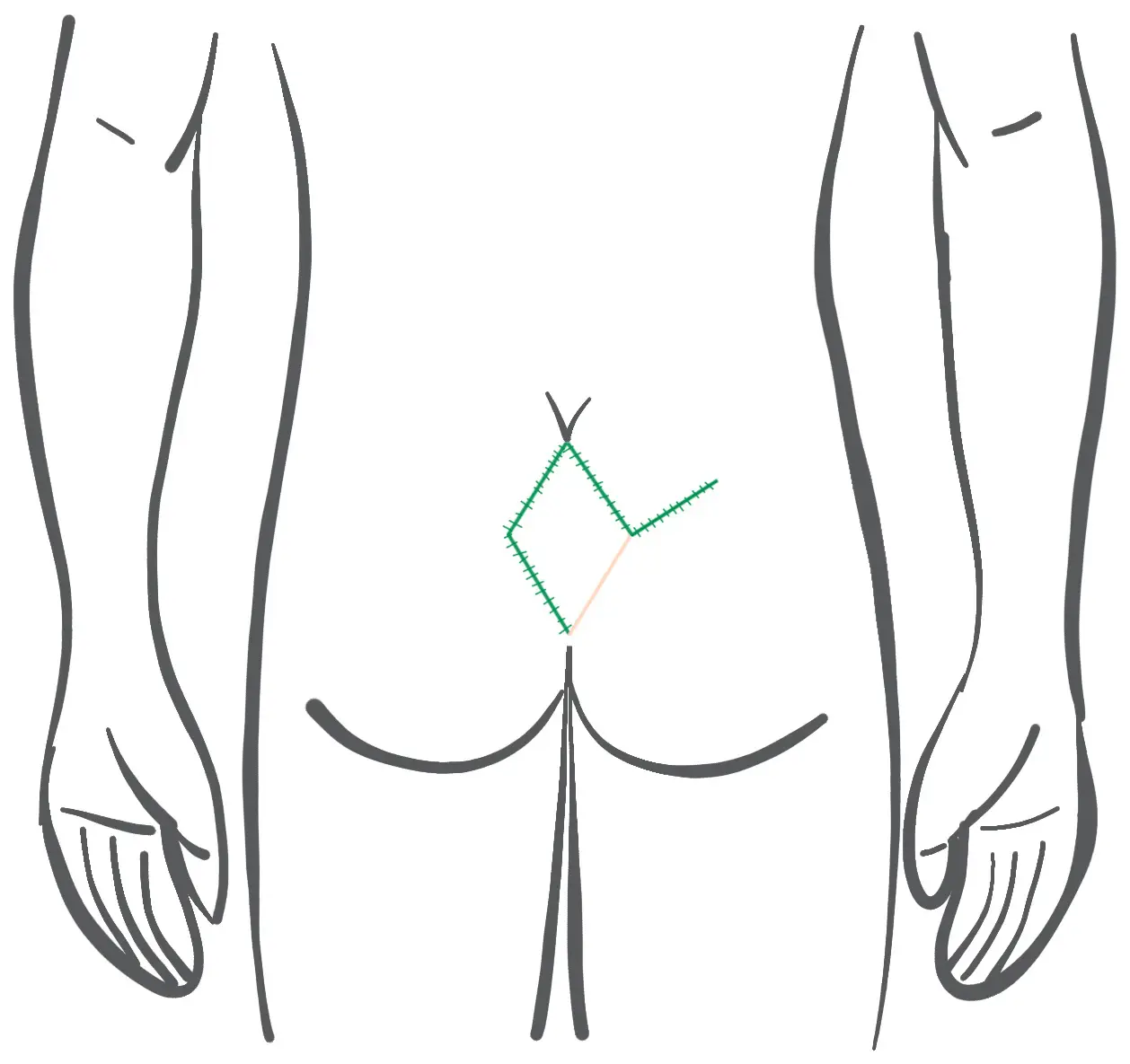
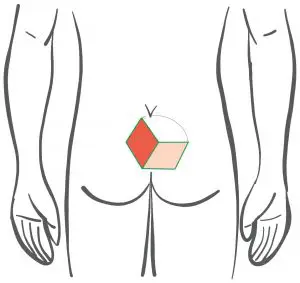
Before: Planning of the lobes - plastic to Limberg with rhomboid cut
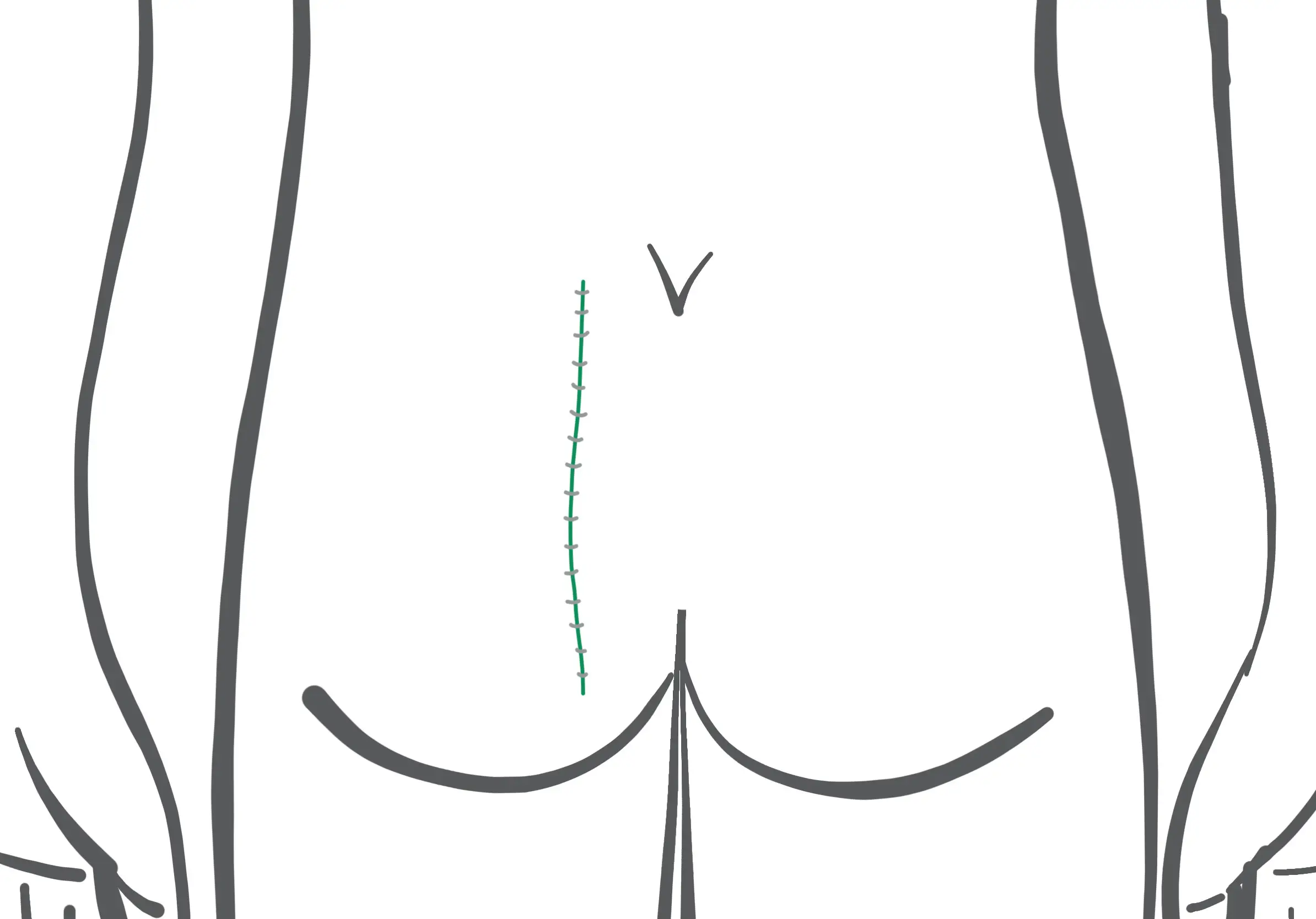
After: Course of the skin suture at Limberg Plastik (the suture lies in the midline!)
Operation Limberg OP
- General or spinal anaesthesia (spinal anaesthesia), in-patient treatment and abdominal positioning
- Cut-out and rotational lobes are rhombus-shaped (i.e. all sides have the same length, unlike the "rhomboid")
- The respective opposite internal angles are 60° and 120°.
- The rue containing the fistula is cut out down to the periosteum of the coccyx and the gluteal fascia.
- A suction drainage is inserted.
- The pedunculated rhombus flap is relocated to the midline wound and sutured in 2 layers.
- The donor site of the flap is closed by a diagonal suture.
- For 10 days, the patient is positioned on the side only .
- Then the skin threads are removed.
- Shaving and showering was recommended.
- If the course is uncomplicated, healing is then achieved.
- Here you will find an illustrative presentation by the Swiss surgeon Prof. Hetzer.
Often the Limberg sculpture is performed as shown by Bozkurt shown. The acute-angled parts of the rhombus in the midline are unfavourable. Furthermore, we often observe that a kind of new gluteal fold forms in the middle of the flap, which predisposes to new "pits" in particular. In publications, a complication rate of 25 % is found, of which almost 10 % require a new operation.
Therefore, if this technique is used, sufficient displacement to the side would have to be ensured, as shown schematically in the pictures below(Wysocki 2019). Even when performed correctly, one is not safe from true recurrences. In the case of anal recurrences, this shift to the side is often not possible at all.


Limberg OP - when do we use the method?
- Never, because there are better alternatives in almost all situations
- The technique may perhaps be an emergency solution if openings are found extremely close to the anus that cannot be closed in any other way. In this case, one would prefer an "inverted" Limberg flap as described by Ahmad et al.
Pro
Even large defects can be closed
In principle possible at any localization
- Good primary cure rates
Contra
- Increased complication rate and re-operation rate compared to Karydakis or Cleft Lift
Unfavourable cosmetic outcome with deformed body contour, lower patient satisfaction in studies
Frequent recurrences (type IV a) when used in the midline
Often formation of numerous "pits" in the new midline with type II a recurrences. Therefore laser epilation is highly recommended if Limberg surgery has already been performed.
Other: Rarely used techniques of plastic reconstruction
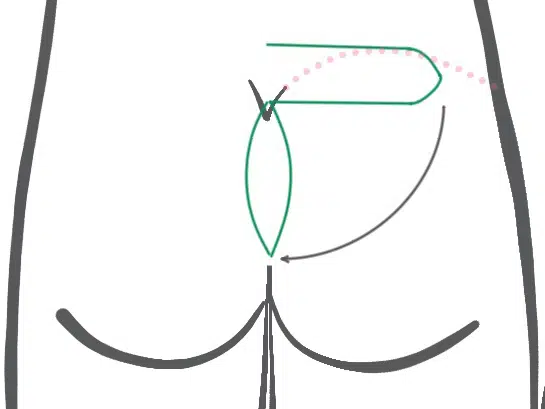
Paraspinal transposition flap
A cranial ("top") pedicled fasciocutaneous flap is pivoted into the midline defect by rotation. The flap, first described by Gupta in 2014, is supplied by the perforator blood vessels L5 and/or S1.
A study from Egypt found a rate of minor complications of 25% and a recurrence rate of just under 4%. Advantages of this flap are said to be its origin far from the midline and rotation from transverse to longitudinal. The theoretical disadvantage is the acute-angled insertion at the most difficult anal site.
Parasacral perforator flap
Lorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et ea rebum. Stet clita kasd gubergren, no sea takimata sanctus est Lorem ipsum dolor sit amet. Lorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et ea rebum. Stet clita kasd gubergren, no sea takimata sanctus est Lorem ipsum dolor sit amet.
Keystone Design Perforator Island Flap (KDPIF)
Lorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et ea rebum. Stet clita kasd gubergren, no sea takimata sanctus est Lorem ipsum dolor sit amet. Lorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et ea rebum. Stet clita kasd gubergren, no sea takimata sanctus est Lorem ipsum dolor sit amet.
Our recommendation traffic light
In no case should the following presentation serve as a guide for an uncritical self-treatment. To the best of our knowledge, the recommendations are based on our own experience and selected publications. They do not represent a systematic analysis of available studies. In any case, consult a specialist experienced in wound treatment before use.
Bibliography: Conventional Surgical Techniques for Pilonidal Sinus
Ahmad, M., & Eltayeb, H. (2020). Combined Horizontal Split Gluteus Maximus Muscle and Fasciocutaneous Limberg Flaps for Reconstruction of Recurrent Sacrococcygeal Pilonidal Sinus. Plastic and Reconstructive Surgery Global Open, 8(12)
Athisayaraj, T., Sebastian, B., Alberts, J., & , (2020). WIDE EXCISION AND RHOMBOID FLAP RECONSTRUCTION FOR TREATMENT OF COMPLEX PILONIDAL DISEASE. CASE SERIES AND REVIEW OF LITERATURE. International Journal of Medical and Biomedical Studies,
Bessa, S. (2007). Results of the Lateral Advancing Flap Operation (Modified Karydakis Procedure) for the Management of Pilonidal Sinus Disease. Diseases of the Colon & Rectum, 50(11), 1935-1940-1935.
Bessa, Samer S. "Comparison of Short-term Results Between the Modified Karydakis Flap and the Modified Limberg Flap in the Management of Pilonidal Sinus Disease A Randomized Controlled Study." Diseases of the Colon & Rectum 56.4 (2013): 491-498-491.
Calisir, A., & Ece, I. (2021). Comparison of the Keystone flap and the Limberg flap technique in the surgical treatment of pilonidal sinus disease. Updates in Surgery, 73(6), 2341-2346.
Chaput, B., Herlin, C., Jacques, J., Berthier, C., Meresse, T., Bekara, F., Sinna, R., Boissière, F., Bertheuil, N., & Grolleau, J. (2019). Management of Pilonidal Sinus Disease with the Aesthetically Shaped Parasacral Perforator Flap: Multicenter Evaluation of 228 Patients. Plastic & Reconstructive Surgery, 144(4), 971-980.
Farag, A., Nasr, S., Farag, A., & Elbarmelgi, M. (2020). The Use of Paraspinal Transposition Flap for Recurrent Pilonidal Sinus, a New Histological Basis for Management of Pilonidal Sinus Disease. Indian Journal of Surgery, 82(4), 514-519.
Faux, W., Pillai, S., & Gold, D. (2005). Limberg flap for pilonidal disease: the "no-protractor" approach, 3 steps to success. Techniques in Coloproctology, 9(2), 153-155.
Gupta, S., Chattopadhyay, D., Agarwal, A. K., Guha, G., Bhattacharya, N., Chumbale, P. K., Gupta, S., & Murmu, M. B.. (2014). Paraspinal transposition flap for reconstruction of sacral soft tissue defects: a series of 53 cases from a single institute. Asian spine journal, 8(3), 309-314.
Hetzer, F. (2021). Modified Limberg flap in pilonidal sinus. coloproctology
Jahan, N., Rahman, M., Roy, S., Islam, S., Alam, M., Ahmed, T., Rahman, C., & , (2021). Limberg Flap Procedure for Managing Sacrococcygeal Pilonidal Sinus Disease: our Experience. Journal of Dhaka Medical College,
Kim, J., Nam, S., Park, E., Choi, C., Cha, H., & , (2021). Surgical Treatment of Sacrococcygeal Pilonidal Sinus with a Leaf Flap. Journal of Wound Management and Research,
Müller, K., Marti, L., Tarantino, I., Jayne, D. G., Wolff, K., & Hetzer, F. H. (2011). Prospective analysis of cosmesis, morbidity, and patient satisfaction following Limberg flap for the treatment of sacrococcygeal pilonidal sinus. Diseases of the colon and rectum, 54(4), 487-494.
Roatis, M., Georgescu, A., & , (2020). Rhomboid Flap vs. Keystone Perforator Island Flap (KPIF) in the Treatment of Pilonidal Sinus Disease: Comparison of Short-Term Results. International Journal of Clinical Medicine
Sarı, R., Akbaba, S., Gündoğdu, R., Yazıcıoğlu, M., & , (2018). Comparison of the V-Y Flap and Limberg Flap Operations in Pilonidal Sinus Surgery. Turkish Journal of Colorectal Disease
Thapa, P., Maharjan, D., Ghimire, R., Shrestha, S., & , (2017). Modified Limberg Flap for Pilonidal Sinus. Nepal Journal of Dermatology, Venereology & Leprology
Turan, A. (2007). A New Flap for Reconstruction of Pilonidal Sinus Lumbar Adipofascial Turnover Flap. Annals of Plastic Surgery, 58(4), 411-415.
Yildiz, A., Yildiz, A., Baris Turhan, V., Kucukdiler, E., Karacan, E., & , (2020). Karydakis Flap Reconstruction for Pilonidal Disease. Acta Scientific Medical Sciences
