Which doctor to see for pilonidal sinus: 10 key points
Welcome to our specialized treatment center. On this page you will find comprehensive information about minimally invasive laser surgery techniques, which offer an effective and less invasive alternative to traditional surgical procedures. This results in numerous benefits, including less pain, faster healing and shorter downtime.
Where are you at the moment?
Diagnosis unclear
Do I really have a Pilonidal sinus?
- What is that?
- What are the typical symptoms of pilonidal sinus?
- What can a Pilonidal Sinus look like?
OP planned
Ignore? Operate? And if so, how?
- Possibilities of treatment without surgery
- Surgical methods
- Advantages of laser treatment and laser surgery
Pilonidal Sinus Recurrence
I've already had surgery. The fistula's back. What to do?
- Why does a relapse occur (recurrence)?
- In which cases can minimally invasive treatment be used for recurrence?
- When is Karydakis surgery recommended?
Pilonidal sinus - What is it?
William James Mayo, founder of the famous Mayo Clinic, first described the clinical picture in 1833. The term fistula (Latin fistula tube, pipe) refers to a tubular duct as a result of chronic inflammation. The term pilonidal sinus (pilonidal sinus, pilonidal cyst, coccygeal cyst, sacral dermoid, dermoid cyst) comes from Hodge 1880 (lat. pilus = hair and nidus = nest).
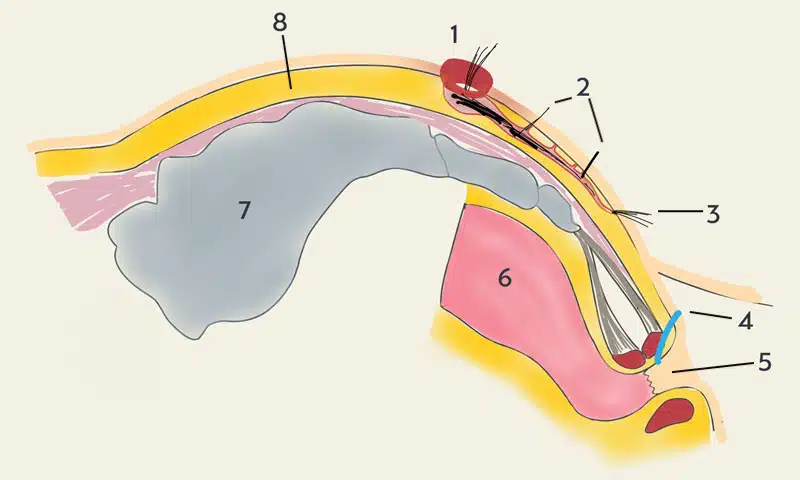
This fistula is only found in the gluteal fold (rima ani). It can be chronic or acute (= abscess, "boil"). Ingrown or impaled hairs lead to an irritation as a foreign body. A protective wall of scar tissue forms, the fistula capsule (foreign body granuloma). The rectum and the sphincter muscle are never affected.
The pilonidal sinus is a simple disease.
1992 George E. Karydakis, Greek surgeon and founder of asymmetric wound closure, Anz Journal of Surgery, 62(5), 385-389.
Unexpected pitfalls and how to avoid them
Why do you need a specialist for a simple illness? What appears to be a minor procedure can have unexpectedly major consequences.
- Long healing time and inability to work
- Extensive and painful wound treatment,
- frequent wound healing disorders
- high relapse rate of up to 57 %(Deutsches Ärzteblatt 2019)
- scarring
- Repeated hospital stays
- Loss of income and career interruption
- Restrictions in sports fitness, weight gain
- Restrictions of body feeling and sexuality
Why patients choose us
1. the entire spectrum of advanced therapy: pit picking, sinusectomy, SiLaC™, EPSiT
Less is more: Based on the pit-picking technique developed in England and popularized in the USA, different variants of this gentle treatment are available.
Pit picking refers to the selective removal of the affected hair roots as skin cylinders with a diameter of 2-5 mm and the cleaning of the fistula tract from deposited hair fragments. The more perfectly this is done, the lower the risk of a new fistula forming.
Pit picking is always combined with treatment of the tubular fistula tract:
- Laser treatment of the fistula from the inside with a fiber optic probe (SiLaC®)
- Precise peeling along the fistula capsule(sinusectomy or fistulectomy).
- Video Endoscopic Surgery (Endoscopic Pilonidal Sinus Therapy EPSiT)
2. cutting-edge medicine for all
Whether you have statutory or private insurance - all our patients benefit from our modern surgical methods. We are fully licensed by the authorities for outpatient surgery and integrated care. Since the beginning of 2024, laser surgery has also been included in the scope of services of all statutory health insurance companies with the introduction of the hybrid DRG. Only laser hair removal is still an IGel self-payer service. Details on billing and reimbursement of treatment costs by insurers can be found here.
Good decisions are based on experience.
John U. Bascom M.D., Pit Picking Pioneer, Eugene/Oregon U.S.A., 1925 - 2013
3. experience from over 7000 operations
Why do you need a specialist for a seemingly simple illness?
Although Pilonidal Sinus is a skin disease, most patients first consult their GP. They are then usually referred to a surgeon.
In Germany, around 50,000 patients are operated on for pilonidal sinus every year. This means that each surgeon treats an average of only 1.4 patients with this condition per year. With such a small number of cases, it is impossible to gain comprehensive experience.
Therefore, it is crucial to choose a doctor who has extensive experience and expertise in modern surgical methods and specializes in the treatment of Pilonidal Sinus. Don't just choose the closest hospital, the quickest appointment or the doctor with the best overall reputation. Choose the best doctor for your specific problem!
7202
Operations (as at 17.06.2024)
8763
Treatment cases (as at 14.04.2022)
Laser Treatments
Experience in laser therapy and laser surgery since 2012
4. easy appointment scheduling via our online calendar
Making appointments in our practice is particularly simple and flexible.
- In case of acute pain, you can come to us directly at any time after informal registration via mail to info@darmsprechstunde.de - we will treat you immediately.
- If you would like an examination and consultation with time for reflection, you can conveniently arrange a appointment via our online calendar.
- For patients who want to save time, we offer the all-in-one appointment: Send us a photo documentation of your complaints in advance and take care of everything you need in just one day. This means you receive the best possible treatment quickly and efficiently.
5. painless, outpatient treatment under local anesthesia directly on the day of the examination
General anesthesia and hospitalization? This is not necessary for our minimally invasive operations. Local anesthesia is completely sufficient. Tumescent anesthesia, a special form of local anesthesia, enables comfortable and safe treatment.
Have you had bad experiences with local anesthesia? We can reassure you. In 99.9% of cases, we still manage to provide pain-free treatment using this method.
We only use general anesthesia in rare cases where local anesthesia is not effective enough and for more complex reconstructive procedures. We perform these procedures in our Iatros Clinic outpatient surgery center. Here too, you can usually return home after a short period of monitoring.
In the first two weeks, you will usually only take painkillers such as ibuprofen if necessary. Stronger painkillers are only needed very rarely.
6. aftercare: wound consultation and via the ArztDirekt app

We will not leave you alone after the operation. A successful operation alone does not guarantee a smooth recovery. We will provide you with detailed advice on follow-up treatment at your surgery appointment.
With our support, a relative can become your personal wound specialist. We use the secure Doctor Direct Messenger for this purpose.
Our information brochures will tell you what to expect during the healing process.
During the follow-up treatment in the practice, your surgeon will personally take care of the optimal healing process if necessary.
In our wound and laser consultation, your wound will be professionally cared for by a trained and experienced therapist.
7. low risk of complications
Complications during pit picking surgery are extremely rare, and serious problems are an absolute rarity. We can therefore offer this outpatient treatment with a clear conscience to patients who have a long journey home after the procedure.
For your safety and well-being, the surgeon is also available 24/7 by cell phone after the procedure to provide support at any time if required.
8. prospects of success
The modern surgical techniques of pit picking and sinusectomy have proven to be superior methods for the treatment of coccyx fistulas. With success rates of over 90 %, they are clearly the better alternatives to conventional procedures. In comparison, traditional operations such as the "Metzger" operation have a high recurrence rate of up to 40 %.
9. recurrence prophylaxis through laser epilation
Studies show that laser hair removal in the affected area significantly reduces the likelihood of recurrence. "Laser hair removal has proven to be an effective method to reduce the recurrence rate in Pilonidal Sinus patients," explains Dr. Hofer, founder of the Pilonidal Sinus Center in Munich. A large meta-analysis from the Netherlands confirms: "Patients who underwent post-operative laser epilation were 50% less likely to have a recurrence." This makes laser epilation a valuable part of aftercare for Pilonidal Sinus operations.
10. experiences and ratings
DR. BERNHARD HOFER & FLORIAN LIEBL
Specialists in Visceral Surgery and Proctology - PartG mbB
Brienner Str. 13, D-80333 Munich
- info@darmsprechstunde.de
- Monday - Friday: 08.00 - 13.00 and 14.00 - 18.00
- and by arrangement
- Saturday, Sunday, Holiday : closed
- Please also note our instructions in the title of this website and on our telephone announcement.
By loading the map, you agree to Google's privacy policy.
Learn more
© 2023 Proctology Practice Munich
