The 6-point risk check
Answering the following questions can help you to identify an increased risk of Pilonidal Sinus . If you answer 'yes' to several of these questions, we recommend that you ask your doctor or another trusted person to examine the gluteal fold for signs such as swelling, redness and especially small openings.
- Do you have a lot of body hair?
- Have any close relatives experienced Pilonidal Sinus ?
- Do you often sit for long hours without a break?
- Do you rarely have the opportunity to wash or shower thoroughly?
- Are you professionally exposed to hair, for example as a hairdresser or in contact with animal hair?
- Do you have pain when sitting?
Feelings of shame should not prevent you from seeking professional medical help if you suspect Pilonidal Sinus . Your health deserves it. The chances of a simple solution to the problem are highest in the early stages.

Sedentary life: Health risks of office and school desk
It may sound dramatic, but it is actually unhealthy to sit for hours without a break. This habit not only causes back pain, but also affects your overall health. An analysis of 27 large studies from 2018 found an increased risk of cardiovascular disease, diabetes and even tumors of the intestines and abdomen, as well as an overall shortened life expectancy, the longer you sit every day.
And of course, the sensitive area of the gluteal fold also suffers from prolonged sitting. The unavoidable, constant shifting of weight when sitting can act like a conveyor belt in the buttock crease, transporting unwanted hair to unwanted places - a potentially painful scenario.
Sitting is even more important if an undetected Pilonidal Sinus already exists. The pressure when sitting can functionally close the small fistula openings (pits), which can lead to painful inflammation.

Wondering what you can do?
- Use a height-adjustable desk at your workplace so that you can work standing up from time to time and do something good for your body.
- Allow yourself regular short breaks to move around and stand up.
- When traveling: Drive out of the rest stop more often and walk a few steps, and don't sit crammed into coach class on the plane all the way to Thailand!
- Make your calls standing up to activate your muscles and improve your posture.
- Use the commercial breaks while watching TV to get up, stretch and move around a bit.
- Bring sporting activities back into your everyday life and feel the energy that movement brings into your life.
- Let apps for smartphones and smartwatches motivate you to move more and get your body moving.
Many employers have recognized that working standing up at least some of the time is beneficial to employees' health and therefore provide height-adjustable desks. It also makes sense to think about purchasing such a desk for home offices. Another positive effect is that there is evidence that people work more creatively and purposefully when they don't spend the whole day sitting down.
"Coccyx Pillow"
The coccyx is by no means a useless extension of the pelvic bones. Numerous ligaments and muscles start here. Incorrect posture does not necessarily lead to Pilonidal Sinus, but to pain when sitting. Suitable seat cushions lead to a redistribution of the weight load and can alleviate such pain.
In the aftercare following Pilonidal Sinus surgery, such a cushion can make sitting easier.
Tips for personal hygiene with pilonidal sinus
General body hygiene
You don't normally get a Pilonidal Sinus because you don't wash yourself enough. However, the deepest point of the gluteal fold (in technical terms: rima ani) is often neglected. If hair fragments collect here, they can be massaged into the skin. Moisture and exfoliated horny scales of the skin form a breeding ground for bacteria and clog enlarged pores. So: when showering, hold one buttock to the side and rinse the rima ani thoroughly.
Prevention of inflammation

Pilonidal Sinus and Sport
Despite a Pilonidal Sinus , it is possible to play sports in many cases as long as certain precautions are observed. The choice of sport plays a crucial role. Sports that generate little pressure and friction in the coccyx area, such as swimming or cycling, are often better tolerated. However, it is advisable to always consult with a physician before continuing or starting any sports activity to ensure that there are no risks or concerns in your individual case. Proper care and hygiene of the affected area and wearing loose, non-restrictive clothing can also help minimize discomfort during exercise. In any case, it is important to listen to your body and consult a physician immediately if you experience pain or problems.
Sweating
Although it is repeatedly claimed, there is no evidence that sweat plays a role in the development of pilonidal sinus.
Sweating is a vital mechanism of the human body to regulate body temperature and remove excess heat. Sweat production is regulated by various factors such as physical activity, ambient temperature, emotions and general health.
Sweat consists mainly of water, electrolytes such as sodium and potassium as well as small amounts of urea, lactic acid and immunoglobulin A.
IgA serves to protect the skin and mucous membranes from microorganisms. It has the ability to bind toxins and, in combination with lysozyme, develops antibacterial and antiviral properties.
And what about wound healing? Well, science does not yet have a clear answer. An acidic pH value and IgA in our sweat could actually protect wounds from infection. Research is currently even being carried out into whether synthetic sweat can improve wound healing.
Sweating also stimulates blood circulation and gives the healing process the necessary kick-start.
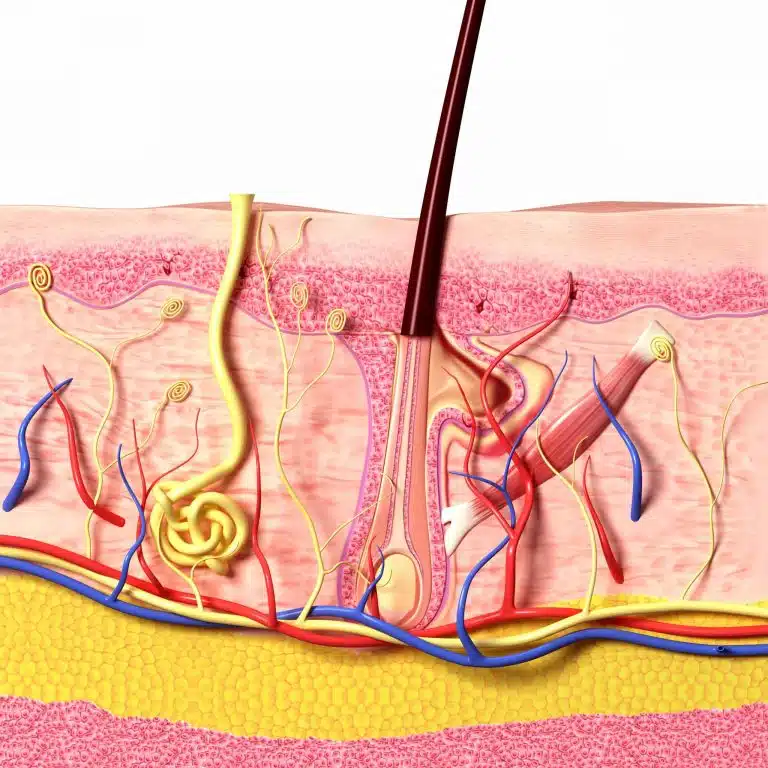
Friction and textile fibers
There is a theory that textile fibers can also penetrate the skin pores through friction and pressure. These penetrated hairs and fibers could trigger a foreign body reaction that leads to inflammation and ultimately to the formation of a pilonidal sinus. However, there are no systematic studies to date that support this assumption. Furthermore, in the almost 7000 pilonidal fistulas that we have operated on so far, I have never been able to identify textile particles that would have been visible to the naked eye or using magnifying glasses. So dust and lint do not seem to be the culprits.
Preventive laser treatment?
If you want to prevent a Pilonidal Sinus altogether, you would have to start early. Probably the first "pits" develop already from the beginning of puberty. Our youngest patients are hardly older than 13 years.
An early, permanent removal of the hair of the gluteal fold by laser would possibly be a causal treatment. Unfortunately, it is not possible to reliably estimate which young people would benefit from laser epilation. Laser epilation is not covered by public health insurance. Several treatments are always necessary. A purely preventive laser epilation therefore seems to me to be justified only in the case of very pronounced hairiness or several family members affected by Pilonidal Sinus .
Publications on the subject of lifestyle
Biddle, S., Bennie, J., Bauman, A., Chau, J., Dunstan, D., Owen, N., Stamatakis, E., & van Uffelen, J. (2016). Too much sitting and all-cause mortality: is there a causal link?. BMC Public Health, 16(1), 1-10.
Dunstan, D. (2010). Too Much Sitting The Population Health Science of Sedentary Behavior. Exercise and Sport Sciences Reviews, 38(3), 105-113.
Eanes, L. (2018). CE: Too Much Sitting: A Newly Recognized Health Risk. AJN: American Journal of Nursing, 118(9), 26-34.
Kennedy, M. (2018). Sitting Our Lives Away. AJN The American Journal of Nursing, 118(9)
Pronk, N. (2011). The Problem With Too Much Sitting A Workplace Conundrum. ACSM's Health & Fitness Journal, 15(1), 41-43-41
Wallace, J. (2015). Effect of Prolonged Sitting and Breaks in Sitting Time on Endothelial Function. Medicine & Science in Sports & Exercise, 47(4), 843-849-843
Our recommendation traffic light
DR. BERNHARD HOFER & FLORIAN LIEBL
Specialists in Visceral Surgery and Proctology - PartG mbB
Brienner Str. 13, D-80333 Munich
- info@darmsprechstunde.de
- Monday - Friday: 08.00 - 13.00 and 14.00 - 18.00
- and by arrangement
- Saturday, Sunday, Holiday : closed
- Please also note our instructions in the title of this website and on our telephone announcement.
© 2024 Proctology Practice Munich

