Pilonidal Sinus: Classification and pictures
On this page about the pilonidal sinus, also known as Pilonidal Sinus , you will find an extensive collection of images to help you better understand your own health problem.
The images on this page are intended to provide you with a visual guide so that you can recognize the characteristic features of Pilonidal Sinus in yourself. Navigate through our picture gallery and find out more about the clinical picture of Pilonidal Sinus. The spectrum ranges from barely visible, dilated hair roots (pits) to finger-thick, cartilage-like hardened fistula ducts.
The images shown on this website may be perceived as distressing or disturbing. We would like to point out that the visual representations of medical conditions are authentic and detailed in order to provide accurate information. The images shown are intended to promote understanding of the diagnosis of pilonidal sinus. However, we would like to point out that the images may not be suitable for everyone and may be perceived as uncomfortable. We recommend viewing the images with caution and seeking medical advice if necessary. These visual representations are not a substitute for individual medical diagnosis or treatment.
The decision to view the images is at the user's own discretion. We accept no responsibility for any inconvenience or distress that may be caused by viewing these images.
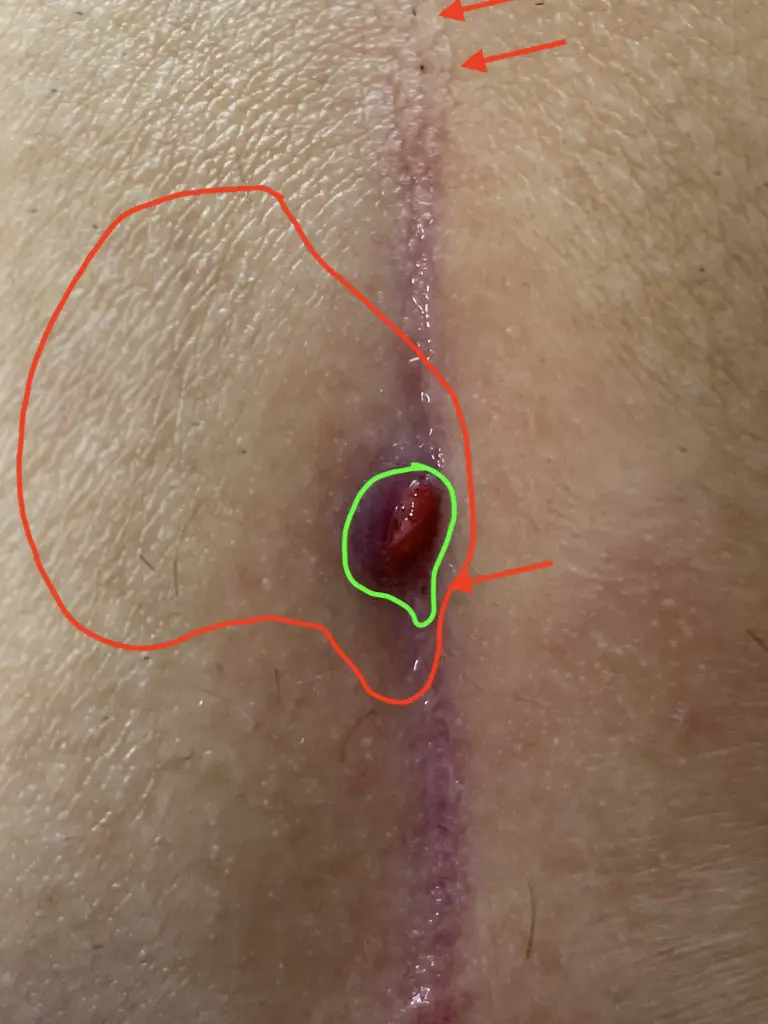
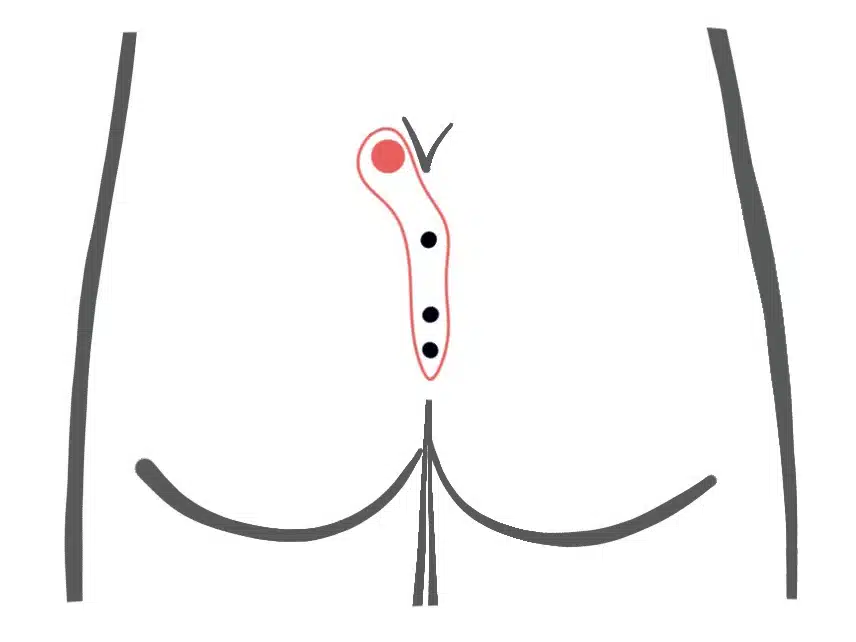
Coccyx abscess (pilonidal abscess)
When an unbearable pain develops overnight: The Pilonidal Sinus usually exists for a long time before it becomes conspicuous by an abscess. The trigger for an abscess is often prolonged sitting or mechanical stress
- on a long-haul flight
- after long car journeys
- in preparation for an examination
- Workout like situps or bench press
Sometimes even the doctor doesn't see much at first glance. With these alarm signs abscess is very likely:
- Increasing pain
- visible bump
- palpable induration
- Redness
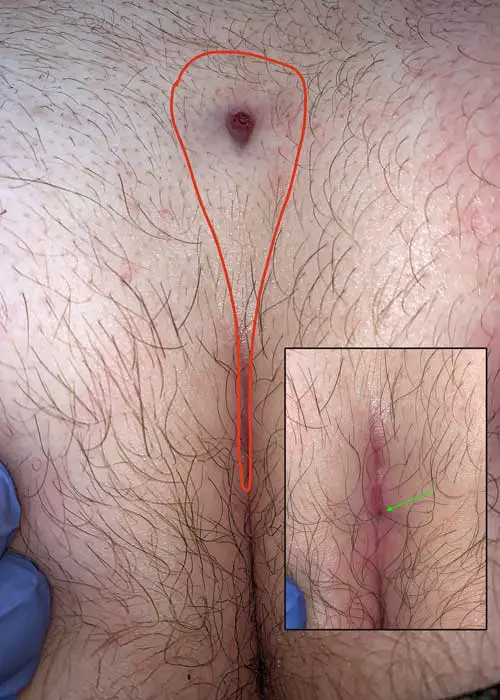
- Asymmetry of the gluteal fold
- Strikingly smooth skin
- If the abscess has ruptured, pus is discharged
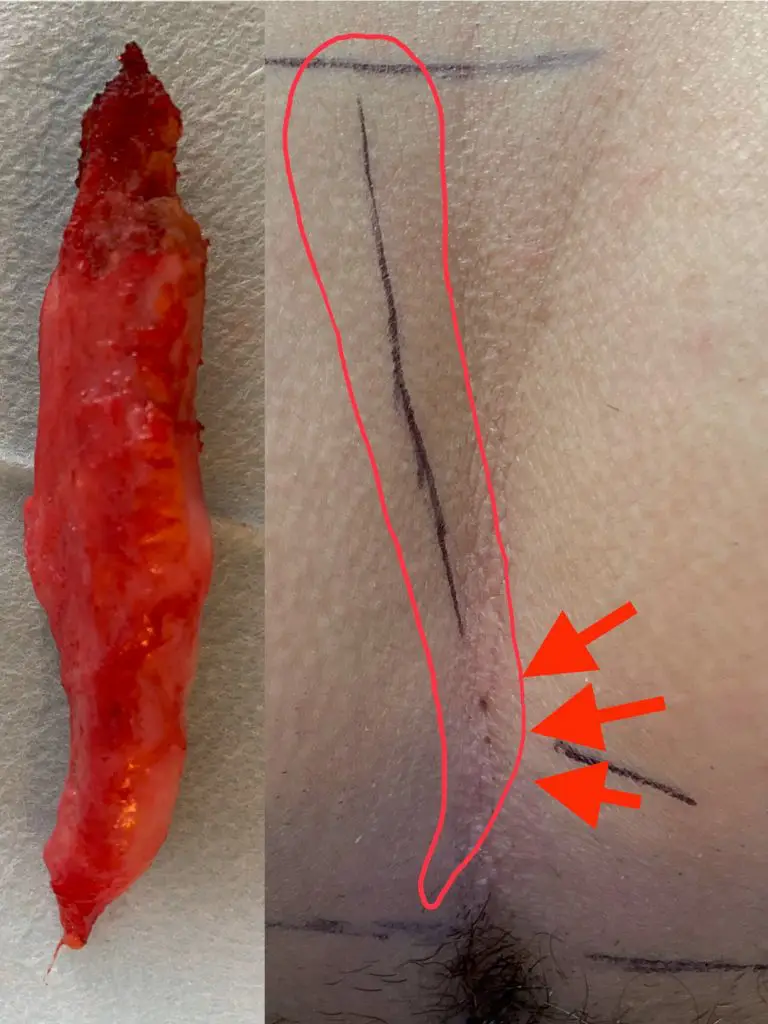
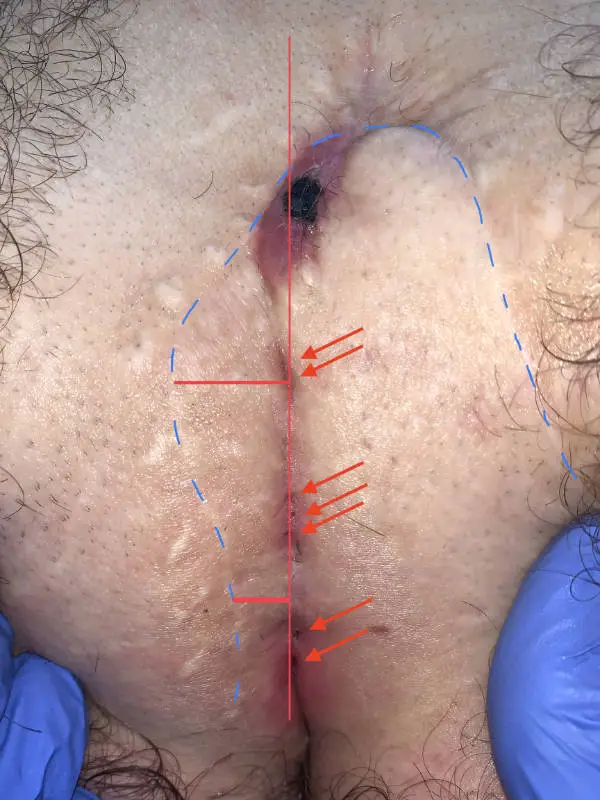
Clinical picture







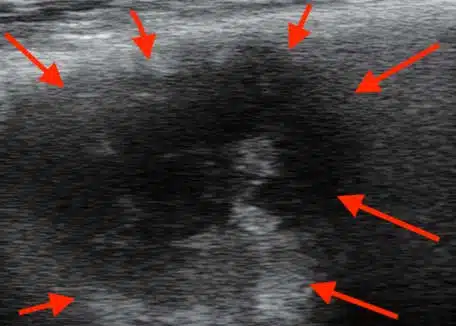
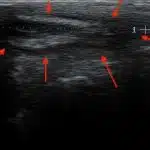
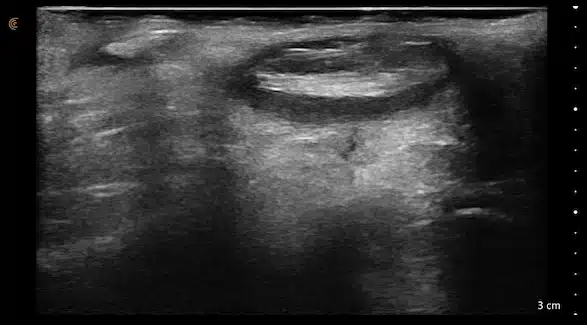
Sonographic image (ultrasound)

Pilonidal abscess: treatment
According to the current guideline 2020, immediate removal of the fistula should not be attempted in the acute situation. Due to the accompanying inflammatory reaction of the surrounding area, too much tissue would always be removed. In addition, it is easy to overlook individual pits in the case of severe swelling.
Ultrasound and palpation findings of a "soft dent in the area of the bump" help to find a favorable location for the Opening the abscess to find.
A small incision provides relief, the pus drains away. The pain quickly subsides.
If the findings are less pronounced, antibiotic treatment may be sufficient in individual cases.
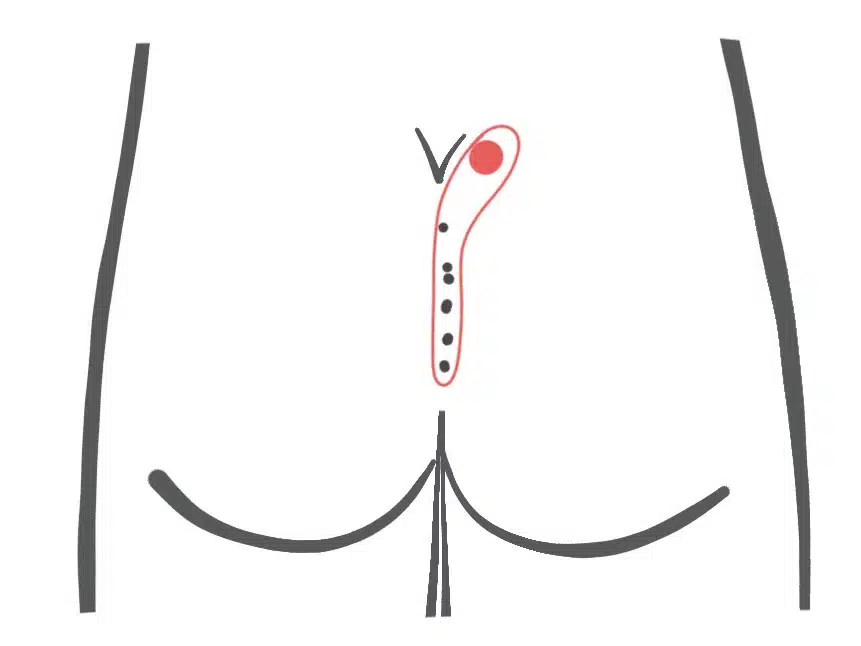
Type I, III and IV according to Tezel
Pilonidal Sinus, primary
With the types I - III of our classification no operation has taken place yet. In its classification, Tezel differentiates between Type I, corresponding to the "blind fistula" with visible openings without symptoms, and Type III with symptoms.
Type I A: Short fistula ≤ 2 cm and maximum 3 primary openings (pits)
The small, uncomplicated Pilonidal Sinus
The small fistula under 2 cm length and with a maximum of 3 pits is sometimes not to be found at first sight.
If the painful point is known, the diagnosis can usually be made with certainty using ultrasound.






First choice treatment: Sinusectomy
Complete, economical triggering with the radio frequency scalpel or the blue 470 nm laser
Alternative: Classic Pit Picking
Pit picking and cleaning of the fistula cavity from hair and skin scales (debridement)
Type I B: Long fistula > 2 cm and and maximum 3 primary openings (pits)
The long, simple Pilonidal Sinus
We see this type of fistula most frequently in our practice.
An expansion of 10 cm and longer is possible. Causal pits are often far down in the gluteal fold and can only be detected after shaving and viewing with magnifying glasses.






1st choice: sinusectomy
With this type of fistula, the fistula tube can be released through small incisions and the overlying skin can be protected. Result: smaller scars and faster healing
Alternative: Pit Picking and SiLaC
For fistulas longer than 4 - 5 cm, the use of the radially emitting laser probe(SiLaC / FiLaC®) be a gentle alternative to sclerosing the fistula with shorter convalescence and a somewhat lower success rate of 75 - 80 %.
Type II A: Long fistula > 2 cm and and ≥ 4 primary openings (pits).
The long, complex Pilonidal Sinus
With an average length of 4 - 5 cm, these fistulas also have numerous or closely adjacent pits. This is often the case in patients who have been pre-operated on with Limberg Plastics. Pits on the side of the midline (off-midline pits) make one think of an acne inversa.





1st choice: sinusectomy
Since these fistulas are often very scarred, often only sinusectomy offers optimal chances of healing. Access is through a small incision at the upper end of the fistula or the narrow excision of the "pimple". The pits can be punched out with 2 - 3 mm or vaporized with laser. The stability of the gluteal fold is maintained.
Alternative: Pit Picking and SiLaC
Laser sclerotherapy can be a sensible alternative for long, slender fistula ducts.
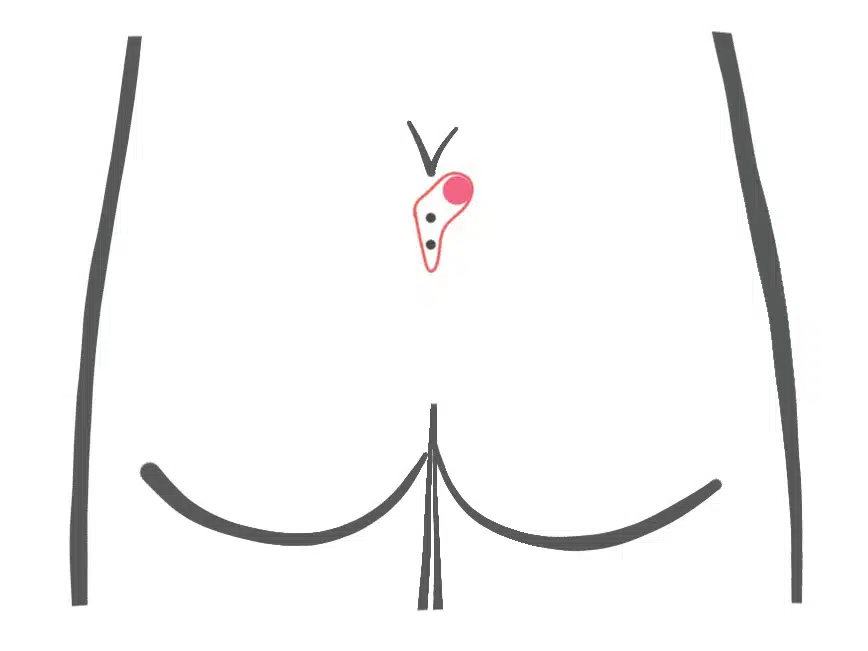
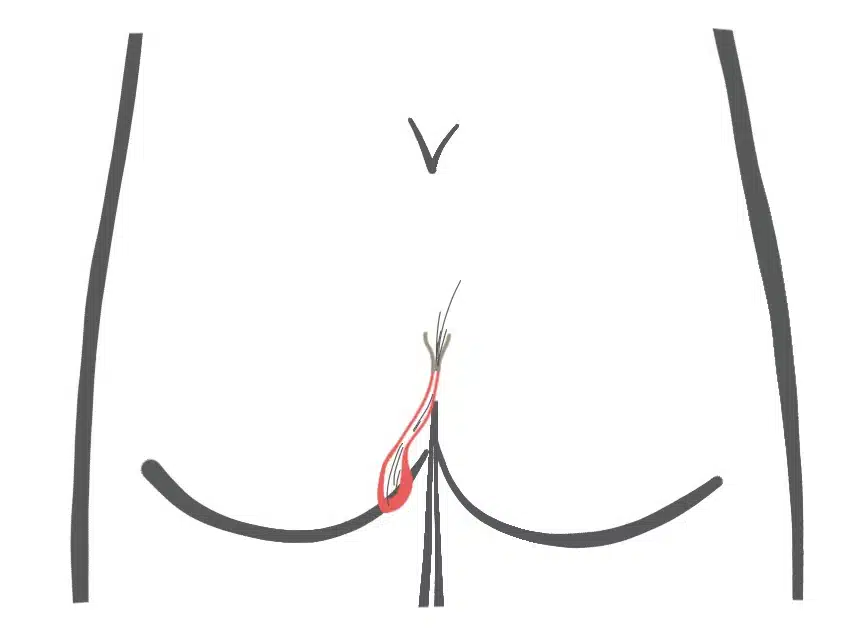
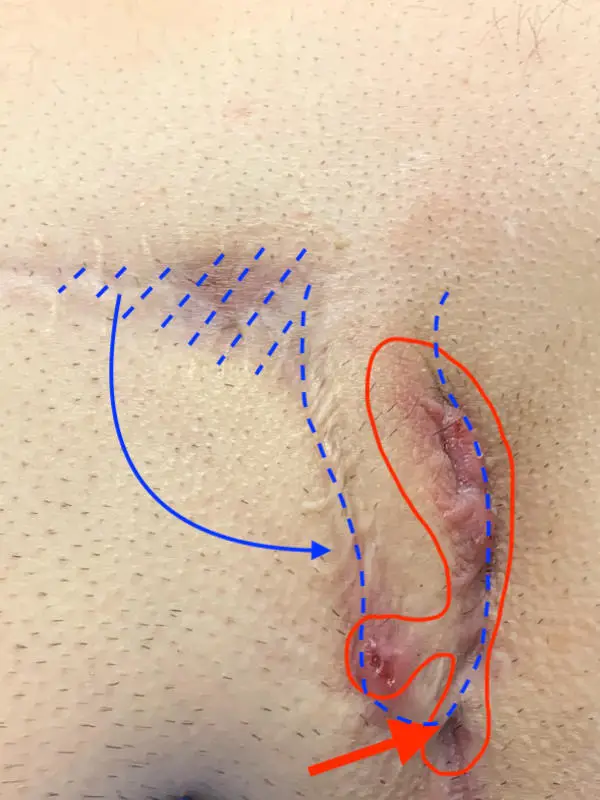
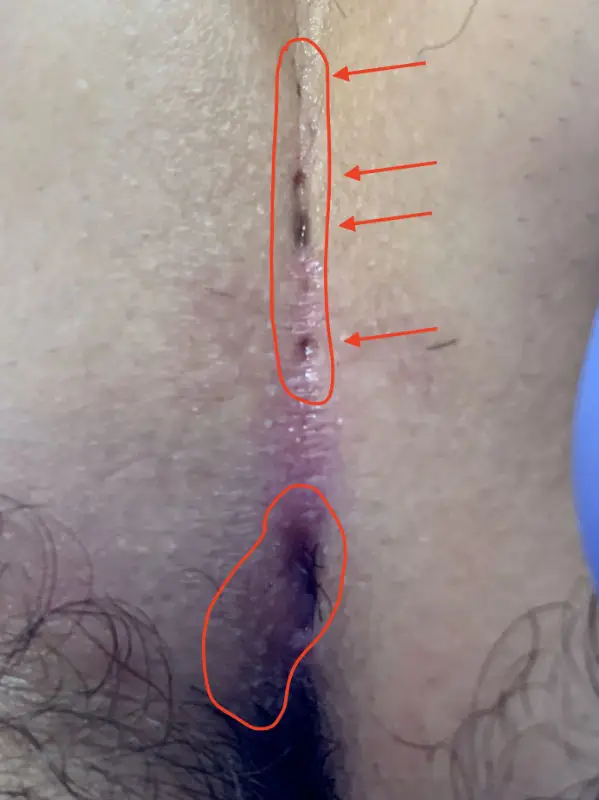
Type II B: Long fistula with blind sac over the lower spine
The flat, large volume Pilonidal Sinus (Type IV according to Tezel)
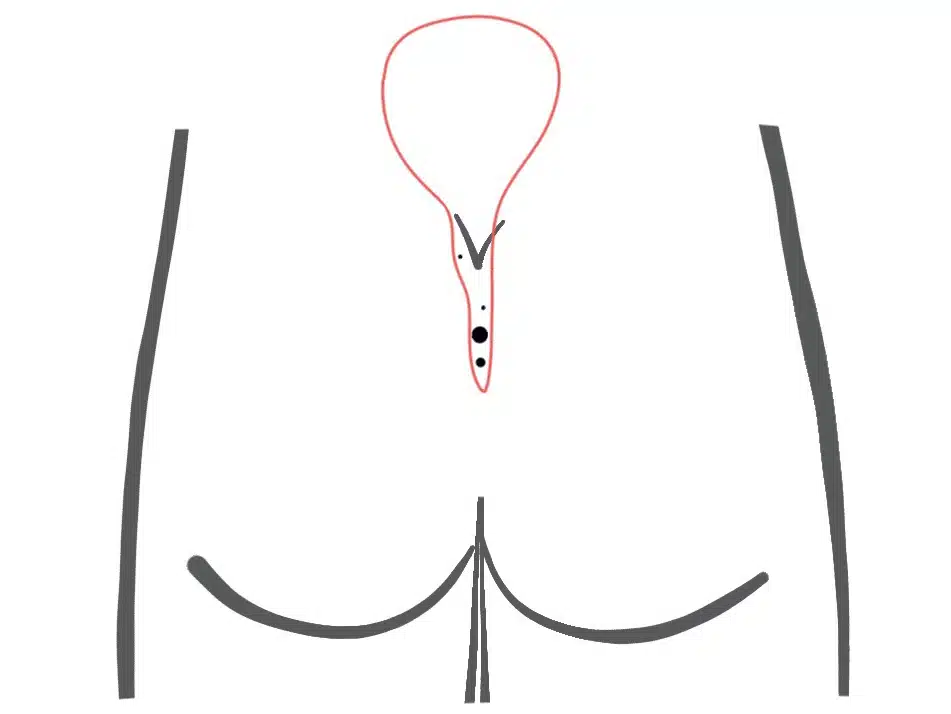
Externally, the extension of this type of fistula is often not obvious. Ultrasound images are therefore particularly important for type II B Pilonidal Sinus . With good planning, unpleasant surprises can be avoided during surgery.



Alternative: complete excision and reconstruction according to Karydakis
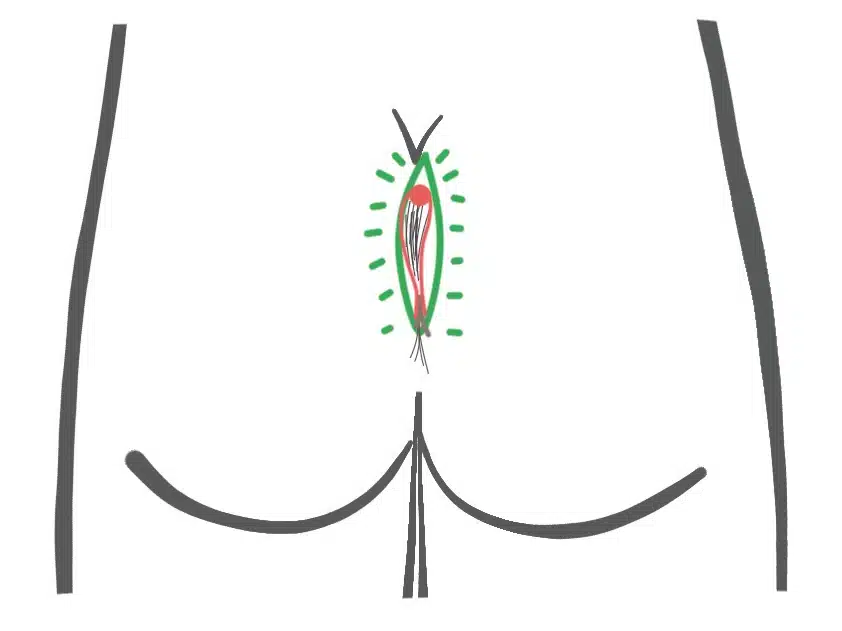
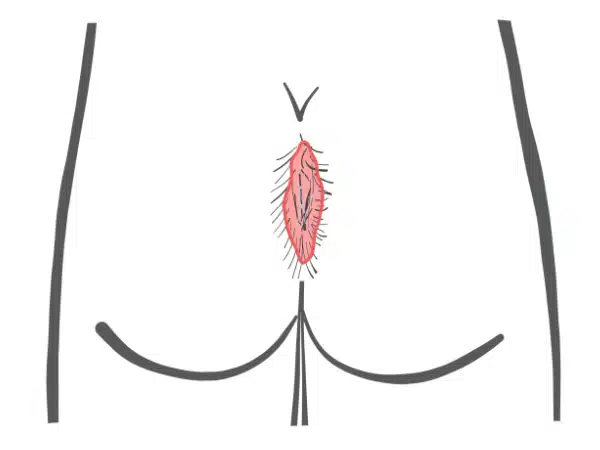
Type III: Secondary fistula after sacral pits
The fistula resulting from a congenital retraction of the skin above the tip of the coccyx
5 % aller Neugeborenen haben eine Einziehung der Haut über der Steißbeinspitze (Sakralgrübchen, engl. sacral dimple). Nur < 0,1 % dieser Kinder entwickeln sekundär eine Fistel. Spinale Fehlbildungen sind extrem selten (Kucera, Wilson). Bei Ausdehnung zur Analregion kann man sie mit Analfisteln verwechseln.




1. sinusectomy
Since these fistulas are often very scarred with a palpable hardened strand and retraction of the skin, only sinusectomy offers good chances of healing.
We would advise against radical surgery or FiLaC/SiLaC for these fistulas. In the area between the tip of the coccyx and the anus, wound healing is often particularly laborious and protracted.
Type V to Tezel
Relapse of a Pilonidal Sinus
If the fistula is present again: The true recurrence, i.e. the reappearance of a pilonidal sinus from the pit to the fully developed fistula, is possible but rare. The types I - III of our classification therefore play less of a role in recurrence.
Our Pilonidal Sinus picture gallery therefore shows the common group IV fistulas. The wound has either never completely healed or pain or openings have recurred after supposed healing. The germ cell for these recurring symptoms are often already in the course of wound healing stored hairs.
The "real" recurrence ...
... is rare!
Wikipedia writes: "A relapse (Latin recidere "to relapse") is the recurrence ("relapse") of a disease or mental disorder."
Recurrence requires that the disease was previously cured. Thus, in a true recurrence, the disease process runs again from beginning to end.
It is basically possible for new pits to form as the cause of a Pilonidal Sinus .
In most cases the recurrence is either a persisting fistula with incomplete removal of the fistula tract or overlooked "pits" or a poorly healed surgical wound ("pseudorecurrence" type IV of our classification).


Type IVa: Tubular pseudo-recurrence
When hairs impale themselves in the scar at the bottom....
This form of fistula can occur after all types of previous surgery. The cause is almost always the ingrowth of hair from the lower pole of the wound. Only later does an opening reappear on the upper edge, when the inflammation has worked its way under the scar.



1st laser sclerotherapy (SiLaC): In the early stages, scraping out the fistula tract and laser sclerotherapy may be sufficient. In this situation, laser epilation is an essential part of the treatment concept.
2. sinusectomy
In many cases, the removal of the fistula tract through the existing openings with radiofrequency scalpel or laser is a goal-oriented treatment.
3. excision and Karydakis plastic
Alternatively we recommend the asymmetrical closure according to Karydakis.
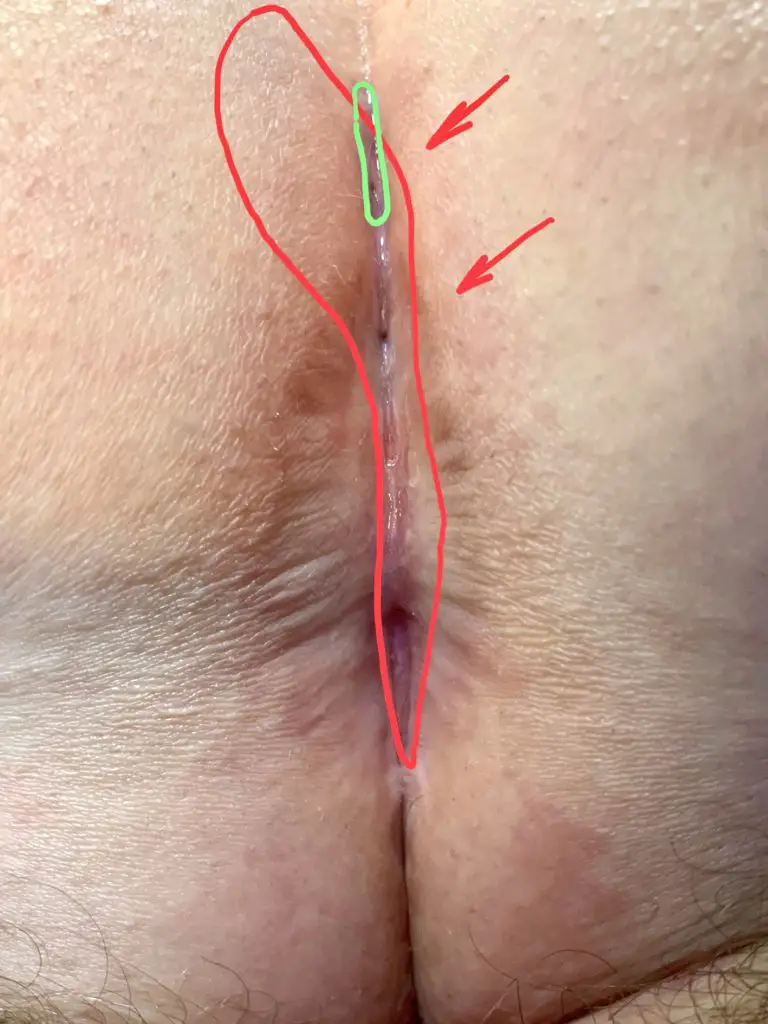
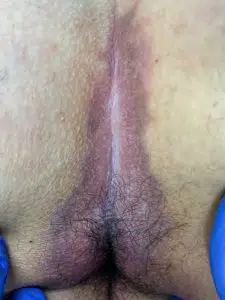
Type IVb: spindle-shaped or oval pseudo-relapse
If loose hair or textile particles prevent healing...
This form of fistula occurs mainly after the spindle-shaped excision with open wound treatment. The cause is the ingrowth of hairs from around the wound. Broken off hairs collect under the skin.
The mechanical stimulus prevents permanent healing. Usually the wound closes again and again, but tears open again at every opportunity. Physical rest can not change this.
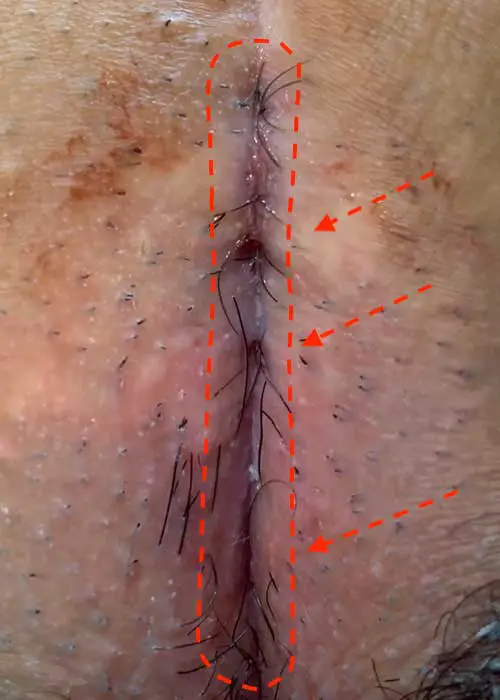



1. sparingly peeling off the hypergranulations ("wild meat"), taking the trapped hair with the Dios Blue Laser Close shaving in the post-treatment and laser epilation ensure the treatment result.
2. excision and Karydakis plastic
Alternatively we recommend the asymmetrical closure according to Karydakis.
Pilonidal Sinus and cancer - Can a pilonidal sinus become malignant?
Rare, but life-threatening...
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.

Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Healing process (before - after - Pilonidal Sinus pictures)
Finally, we show Pilonidal Sinus pictures of the course of treatment. Basically, each "case" is an individual case, so that the procedure and treatment result are not easily transferable to future treatments. However, you can see that very good treatment results are possible without radical surgery.
Patient 26 years, no previous surgery, type I A fistula


Patient 30 years old, no previous surgery, type II A fistula




Patient 37 years, type I B fistula as mixed form to acne inversa




Patient 26 years old, type I B fistula with 2 pits, first presentation with abscess




Patient 38 years, longstanding known fistula type II A


Patient 24 years, no previous surgery, type II A and III combined

Patient 23 years old, type IV B fistula, first presentation with non-healing wound


Patient 35 years, type IV B fistula, previously 3 operations in 10 years, wound never healed


Patient 17 years, recurrence after Limberg plastic surgery



Patient 28 years, double fistula

Patient 25 years, type II A fistula


Patient 19 years, type II A fistula


Inflammation above the coccyx, but no Pilonidal Sinus
Not every wound or inflammation in the buttock crease is a Pilonidal Sinus. After so many sinus pilonidalis images, here are illustrations of some important differential diagnoses.
Rhagade of the Rima ani (butt fold)
Superficial tears
A raghade is a wound that looks like a tear or a cut. It always affects only the most superficial layer of the skin, the epidermis.
In patients who have already undergone surgery using the "Metzger" method, the cause is probably a lack of stability of an inelastic scar in the face of the strong shear forces.
But even in patients who have never been operated on before, such raghaden occur. The most common form of psoriasis is then a limited form of psoriasis.
Rhagades can lead to a usually low secretion of yellowish secretion (fibrin), so that one mistakenly suspects a suppurating fistula.
The treatment is conservative. In acute phases cortisone and antibacterial creams (e.g. Fucicort®) help.


Infected atheroma (groat pouch)
Inflamed sebaceous gland
An atheroma is a cystic accumulation of a pasty secretion. The cause is a clogged gland of the skin. It can remain asymptomatic for a long time, and then become inflamed for no apparent reason.
In these cases, the inflammatory reaction of the surrounding tissue often reaches a magnitude that is much larger than the cyst itself. A kind of pus pimple is sometimes found centrally in the "bulge". Typical pits in the midline are missing.
These cysts can also be removed through relatively small incisions, the probability of a relapse is lower than with the typical Pilonidal Sinus.

Acne inversa
Acne inversa (older name hidradenitis suppurativa) is a chronic fistulous disease that is found preferentially in the axilla, groin, perianal region and skin fold under the female breast.
The frequency (prevalence) is given as 0.05% to 4.1%. The average time from the first symptoms to diagnosis is 7.1 years.


The disease begins with inflammation of the hair follicles by lymphocytes, followed by loss of the sebaceous glands, congestion of the hair follicle, and finally bursting (follicle rupture) with penetration of the contents into the subcutaneous tissue.
The inflammation spreads without regard to anatomical barriers and the typical picture of numerous fistula openings with varying degrees of scarring, confluent fistulas and progressive tissue destruction develops. In the tissue, the inflammatory hormones interleukin-1 (IL-1), tumor necrosis factor (TNF) and many others are elevated.
There is a certain genetic disposition for these fistulas, in which a misregulation of the immune reactions is assumed.
On the adjoining acne inversa pictures one can see the typical scarring, lateral openings and branching of the disease formerly also called hidradenitis suppurativa.
99% of all patients with acne inversa who have ever entered my practice are smokers. A cure for this systemic disease is only possible after smoking cessation. Surgery can remove existing foci and relieve abscesses, but cannot prevent recurrences.
New treatment approaches are laser treatment, the LAIGHT therapy, which was investigated in studies at the University of Mainz, and laser ablation.
There is often no way around a conventional excision.
Lichen (ruber) planus
Lichen ruber planus is a not so rare (prevalence 0.5 %) autoimmune disease of the skin and sometimes also of the mucous membranes. It is characterised by the formation of slightly raised skin rashes from coalescing individual lesions (papules). Net-like, whitish deposits, the so-called Wickham's stripes, can be seen on the surface.
The cause is still unclear, sometimes there is a connection with liver disease and stress. There is often a pronounced itching. In 90 % of patients, the disease heals within 2 years. Cortisone and other immunomodulators (Protopic®) are used therapeutically, sometimes also first-generation antihistamines. In some patients, once-weekly administration of enoxaparin (a heparin-like drug used for thrombosis prevention) is effective.
Anal fistula
A Pilonidal Sinus practically never finds connection to the anal canal or intestine. Here you will find information about anal fistula and the treatment of anal fistula.
